Your Guide to the Rivermead Concussion Questionnaire
Dec 2, 2025
The Rivermead Post-Concussion Symptoms Questionnaire (RPQ) is one of the most trusted tools in brain injury recovery. It's a self-report questionnaire that helps measure the severity of physical, cognitive, and emotional symptoms after a concussion. In essence, it takes subjective feelings—like headaches or forgetfulness—and translates them into objective data clinicians can use to track recovery.
Decoding the Concussion Symptom Map

After a concussion, a person’s world can feel chaotic and confusing. Symptoms like dizziness, fatigue, and irritability are invisible challenges, making them incredibly difficult to explain and even harder to measure. Think of the Rivermead questionnaire as a detailed "symptom map" designed to bring clarity to this confusion.
This vital tool helps chart the precise location and intensity of a patient's post-concussion struggles. By asking individuals to rate 16 common symptoms, it transforms personal feelings into a structured, numerical score that everyone can understand.
Turning Subjective Feelings into Objective Data
The main goal of the RPQ is to create a solid, reliable baseline of a person's condition right after the injury. Instead of a patient just saying, "I feel dizzy," they can rate their dizziness on a scale from 0 (not a problem at all) to 4 (a severe problem).
This simple shift provides clinicians with concrete data points to:
Establish Severity: Get a clear picture of the injury's immediate impact. For example, a high initial score quickly signals the need for significant rest and activity modification.
Track Progress: Compare scores over time to see if symptoms are improving. A declining score is an actionable signal that the current recovery plan is working.
Inform Treatment: Make data-driven decisions. If a patient's scores for "noise sensitivity" remain high, it's a clear insight to recommend environmental changes, like using noise-canceling headphones.
This process is a crucial piece of the puzzle. For a deeper look at how clinicians gather this kind of information, you can explore our guide on what is a neuropsychological assessment.
Why This Symptom Map Matters
The RPQ's real power is in its simplicity and standardization. It creates a common language for patients, their families, and healthcare providers to talk about the recovery journey. A single score can summarize a complex jumble of symptoms, making it much easier to communicate progress or setbacks.
The Rivermead Concussion Questionnaire quantifies the often-invisible burden of post-concussion symptoms. It provides a clear, consistent metric for monitoring recovery and bridges the gap between a patient’s internal experience and a clinician’s need for objective measurement.
First developed back in 1995, its effectiveness is well-established. For example, data from one multinational study showed the average total RPQ score for people with mild traumatic brain injury (TBI) was 14.7, showing a symptom load that's clinically significant. This really highlights the tool's ability to capture meaningful data across different groups.
At Orange Neurosciences, we know that turning subjective experiences into measurable data is the first step toward effective, personalized care. To learn how our tools can help you achieve this, visit our website or send us an email to connect with an expert.
How to Score the RPQ with Practical Examples
Scoring the Rivermead Concussion Questionnaire is surprisingly simple, designed to take a patient's lived experience and translate it into a single, meaningful number. This score gives clinicians, patients, and their families a clear baseline to track recovery from.
The questionnaire walks through 16 common post-concussion symptoms. For each one, the person is asked a crucial question: How much of a problem has this symptom been over the last 24 hours compared to before the injury? This comparison is the key to isolating the symptoms that have shown up or gotten worse because of the concussion.
The rating scale itself is an intuitive 0-to-4 system.
Understanding the 0-4 Rating Scale
Every number on the scale has a specific meaning, which helps standardize how a patient reports their symptoms. This consistent framework is what makes comparing scores over time so reliable—a cornerstone of good concussion management. To really appreciate why this works, it’s helpful to understand the principles of test-retest reliability statistics, which are all about confirming a tool's consistency.
The scoring system is broken down into five distinct levels, making it easy for both the clinician and the patient to understand the severity of each symptom.
Below is a table that not only defines each score but also provides a real-world example using the common symptom of headaches. This helps put the abstract numbers into a concrete context.
RPQ Symptom Scoring Breakdown with Examples
Score | Description | Practical Example for 'Headaches' |
|---|---|---|
0 | Not experienced at all | "I haven't had any headaches in the last 24 hours." |
1 | No more of a problem | "I get occasional headaches, but they're no different than before my injury." |
2 | A mild problem | "I've had a dull headache that's annoying but hasn't stopped me from working." |
3 | A moderate problem | "My headache has been constant today, making it hard to focus on my tasks." |
4 | A severe problem | "The headache is so bad I had to lie down in a dark room and couldn't go to school." |
This scoring structure allows for a clear and consistent method of quantifying what are often very subjective experiences.
To get the final score, you just add up the ratings (0-4) for all 16 symptoms. The total will fall somewhere between 0 (no symptoms) and a maximum of 64 (severe symptoms across the board).
Practical Scoring Example One: The Student-Athlete
Let's imagine "Alex," a 17-year-old hockey player who took a hard hit in a game. Two days later, he sits down with his athletic therapist to fill out the RPQ.
Alex points to a few key symptoms that are new or much worse since the hit:
Headaches: 4 (Severe problem)
Feelings of Dizziness: 3 (Moderate problem)
Noise Sensitivity: 3 (Moderate problem)
Light Sensitivity: 4 (Severe problem)
Poor Concentration: 3 (Moderate problem)
Taking Longer to Think: 2 (Mild problem)
Fatigue: 3 (Moderate problem)
He marks all nine other symptoms as 0 or 1, since they're either not there or just his normal baseline.
We add up his scores: 4 + 3 + 3 + 4 + 3 + 2 + 3 = 22. This score of 22 isn't just a number; it’s a clear snapshot of his symptom load. This is an actionable insight for the therapist, immediately triggering the team's concussion protocol, which includes complete rest from physical and cognitive exertion.
Practical Scoring Example Two: The Adult Post-Accident
Now, meet "Maria," a 45-year-old office worker who was in a fender bender. She didn't hit her head, but the whiplash left her feeling "off." A week later, she's at her family doctor's office.
Her RPQ responses paint a different picture:
Headaches: 2 (Mild problem)
Sleep Disturbance: 3 (Moderate problem)
Being Irritable: 2 (Mild problem)
Feeling Frustrated or Impatient: 3 (Moderate problem)
Forgetfulness, poor memory: 2 (Mild problem)
Blurred Vision: 2 (Mild problem)
Maria scores 0 or 1 on the other ten symptoms.
Her total score is 2 + 3 + 2 + 3 + 2 + 2 = 14. While that’s lower than Alex's score, 14 is still clinically meaningful. It validates her feeling that something isn't right and provides her doctor with an actionable roadmap. The high scores for sleep and irritability point to specific interventions, such as recommending sleep hygiene strategies and providing resources for stress management.
A final RPQ score is more than just a number; it’s a story. It captures the unique combination of physical, cognitive, and emotional challenges a person is facing, creating a clear starting point for their recovery journey.
These examples show how the exact same questionnaire can tell two very different post-concussion stories. The final score isn't an abstract data point—it's a powerful summary that helps guide what comes next. By using the RPQ consistently, clinicians can track these scores over time to see what’s working and make smarter decisions.
Want to learn how our digital tools can simplify tracking symptoms and cognitive function? Visit our website to see how we can support your clinical workflow, or email us to schedule a demo.
Interpreting Scores for Clinical Decisions
Once a patient finishes the Rivermead Concussion Questionnaire, you're left with a single number. But that score is so much more than a data point—it's a critical piece of the puzzle that helps guide the entire recovery process. The real magic of the RPQ happens when you translate that number into actionable clinical insights.
A patient's score gives you an immediate snapshot of their symptom severity. This allows you to quickly categorise their condition and start building a suitable management plan. Established score thresholds act like signposts, pointing toward the level of care and intervention a patient might need and helping take the guesswork out of the initial assessment.
This simple flowchart shows how an individual symptom rating contributes to that final, interpretable score.
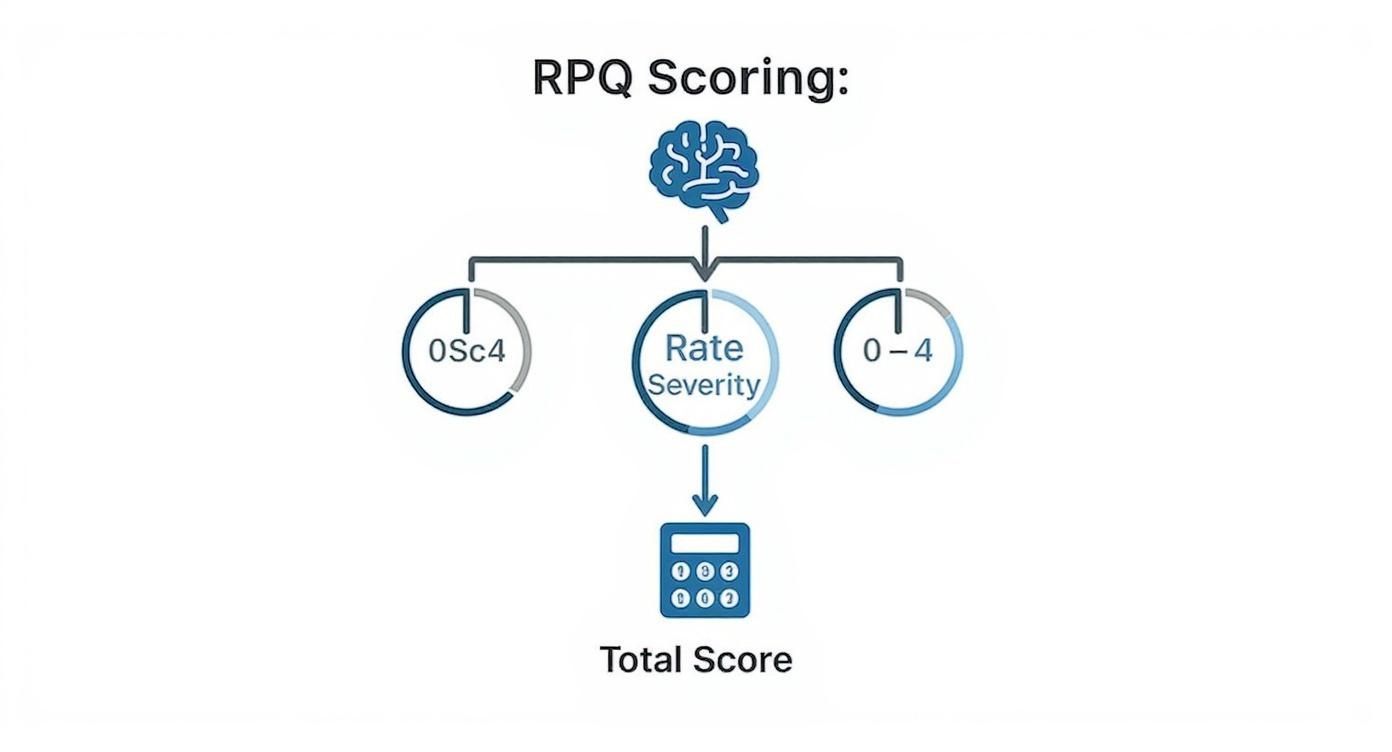
As you can see, each rating is a building block toward a final score that helps shape your clinical decisions.
What the Numbers Mean
Different score ranges on the RPQ point to different levels of symptom burden. This helps frame the clinical conversation and sets realistic expectations for recovery. While every patient’s journey is unique, these general guidelines are a great starting point for interpreting initial results.
Scores Below 12: This often suggests minimal post-concussion symptoms. The patient might be dealing with mild issues, but they are unlikely to get in the way of daily activities. Actionable Insight: Monitor the patient, but active rehabilitation may not be needed. Educate them on gradual return to activity.
Scores from 13 to 35: This range typically indicates a mild to moderate symptom load. A patient here is probably facing noticeable challenges that affect their work, school, or home life. Actionable Insight: This is a trigger to develop a formal recovery plan, which may include physical therapy, academic accommodations, or specific lifestyle changes.
Scores Above 35: This signals a significant, and potentially severe, symptom burden. These individuals may be experiencing functional limitations that demand more intensive support and a comprehensive rehabilitation strategy. Actionable Insight: Consider immediate referral to a multidisciplinary concussion clinic or specialists for comprehensive care.
These thresholds provide a solid foundation for discussing the injury's impact. However, the true strength of the RPQ isn't just in a single score—it’s in tracking how that score changes over time.
The Power of Tracking Scores Over Time
A single RPQ score is a snapshot; a series of scores tells a story. When you monitor these numbers over weeks or months, you get clear, motivating evidence of a patient’s recovery path. This longitudinal tracking is absolutely essential for making informed clinical decisions and tweaking treatment plans as needed.
Consider this practical example: A patient's initial RPQ score is 30. After six weeks of therapy, their score drops to 18. This isn't just a number—it's powerful proof that the treatment is working. This data provides an actionable insight: continue the current therapy and use the score reduction to motivate the patient.
On the flip side, a score that stays stubbornly high—or even climbs—is an important clinical red flag. If a patient’s score hovers around 28 for several weeks without improvement, this is an actionable signal to re-evaluate the treatment plan. It might be time to refer them to a specialist, like a neuropsychologist or a vision therapist, to dig deeper.
The RPQ is instrumental in monitoring how symptoms evolve, helping distinguish early symptom clusters from the more persistent ones that can linger. For instance, scores between 16 and 35 may point toward post-concussion syndrome, while scores above 35 can predict moderate to severe functional limitations down the road.
Since some concussion symptoms can persist for months or even years, the RPQ serves as a vital tool for long-term tracking. It enables healthcare providers to evaluate symptom trends, plan interventions, and accurately assess recovery. This is crucial, as concussion-related impairments can significantly impact quality of life. To find out more about how these challenges can develop, learn more about the long-term effects of concussion in our detailed guide.
By tracking RPQ scores over time, clinicians can transform the recovery journey from a subjective experience into a measurable process. This data empowers both the provider and the patient to set realistic goals, celebrate progress, and make confident decisions about the next steps in care.
Using the Rivermead Concussion Questionnaire effectively means looking beyond that first number. It’s about using data to build a narrative of recovery, guide treatment, and foster clear, compassionate communication every step of the way.
Using the RPQ in Sports Concussion Management
In the high-speed world of sports, a concussion can pull an athlete from the game in a heartbeat. For the athletic therapists and team doctors on the sidelines, managing these injuries demands precision, consistency, and cold, hard data. This is exactly where the Rivermead Post‑Concussion Symptoms Questionnaire has become a trusted tool in modern sports medicine, especially when it comes to the all-important return-to-play decision.
When an athlete’s career and health are on the line, we have to move beyond just asking if they "feel better." The RPQ gives clinicians a standardized way to actually quantify an athlete's symptoms. This isn't just about feelings; it's about turning subjective experiences into objective numbers, which is critical for making safe, evidence-based decisions that put an athlete's long-term health ahead of the pressure to win.
Establishing a Baseline for a Safe Return
The best concussion protocols don't start after an injury—they start before the season even kicks off. Many forward-thinking athletic programs now use the RPQ in the preseason to get a baseline score for every single athlete. It’s a simple step, but its impact is massive.
Think of a baseline score as an athlete's normal, healthy state. When a concussion occurs, clinicians aren't guessing what "normal" looks like; they can compare the post-injury RPQ score directly against that athlete's personal benchmark. The goal becomes crystal clear: the athlete’s score needs to get back to their individual baseline—or as close to zero as possible—before they’re cleared to start the return-to-play process.
This approach strips the ambiguity out of recovery. Instead of relying on gut feelings, the medical team has a tangible target to aim for.
In sports, a baseline RPQ score is like an athlete's personal "symptom fingerprint." A safe return to play is only on the table once their post-injury assessment matches this original, healthy print.
A Practical Return-to-Play Scenario
Let's walk through a real-world example. Picture a university soccer player who takes a hard hit to the head during a match.
Immediate Assessment: On the sidelines, the medical staff pulls out a tool like the Sport Concussion Assessment Tool (SCAT) for the initial evaluation.
Follow-up with RPQ: Within the next 24-48 hours, the athlete sits down to complete the Rivermead questionnaire. Her score comes back as a 25, a huge jump from her preseason baseline of 3.
Monitored Recovery: The athlete rests, and her symptoms are tracked weekly with the RPQ. Her scores tell the story of her recovery: 25 → 18 → 11 → 5.
Clearance for Protocol: Once her score finally drops back down to 3, matching her baseline, the medical team has an actionable data point. This gives them the green light to begin the gradual, step-by-step return-to-play protocol.
This systematic process ensures that no one rushes the decision. The data from the RPQ gives the team objective proof that the athlete's brain has healed enough to safely handle the intense physical and cognitive demands of their sport.
Working Alongside Other Assessment Tools
The RPQ is a team player; it rarely works alone. In any solid sports concussion program, it’s part of a bigger battery of tests, often used hand-in-hand with the SCAT. While the SCAT looks at things like balance, cognition, and neurological function, the RPQ zooms in to provide a detailed, specific picture of the athlete's own reported symptoms.
The synergy between these tools isn't just theoretical. A Canadian research study with 215 athletes showed that RPQ total scores were strongly correlated with SCAT total scores over a 16-week recovery period. This incredibly high correlation (Spearman rho = 0.91) is a powerful confirmation that the RPQ is a reliable partner in a thorough assessment, giving it strong concurrent validity. You can dig into the full study yourself in the Frontiers in Sports and Active Living journal.
By building the RPQ into their standard protocols, sports organizations can make smarter, data-driven decisions that protect their athletes. To get a better sense of how this tool fits into the bigger picture of concussion care, check out our complete guide on the post-concussion symptoms questionnaire.
Ultimately, the Rivermead Concussion Questionnaire helps foster a true culture of safety. It gives medical staff the objective data they need to confidently clear an athlete for return, making sure that their well-being always stays the number one priority.
Common Limitations and How to Address Them
The Rivermead Post-Concussion Symptoms Questionnaire is an incredibly useful tool for putting a number to a patient's symptoms, but it's not the whole story. Like any clinical instrument, it has its blind spots. Understanding these limitations is key to using it effectively and getting a true, holistic picture of a patient's recovery.
Let's be clear: no single questionnaire can capture the full complexity of a brain injury.
A major point to remember is that the RPQ is a self-report measure. The scores hinge entirely on the patient's own perception, which can be swayed by all sorts of things happening in their life.
For example, a patient dealing with a high-pressure job or family stress might rate their irritability much higher, even if the concussion isn't the only cause. Pre-existing conditions like anxiety or depression can also easily colour their responses, skewing the results.
The Challenge of Symptom Overlap
Another big consideration is that the symptoms themselves aren't unique to concussions. This is what we call symptom non-specificity. Many of the 16 symptoms on the list—like fatigue, headaches, or trouble concentrating—are common complaints across dozens of other conditions, from migraines and sleep disorders to chronic stress.
This overlap can really muddy the waters. As a clinician, you have to play detective. Is that high "fatigue" score a direct result of the brain injury, or is it tied to poor sleep habits that were there long before the incident?
The Rivermead questionnaire tells you what symptoms a patient is experiencing. It's the clinician's job to figure out why. The root cause often goes far beyond the concussion itself.
So, how do we navigate these challenges? The best approach is to treat the RPQ as just one piece of a much larger puzzle, never as a standalone diagnostic.
Strategies for a Balanced Assessment
By weaving the RPQ into a broader clinical framework, you can get a far more nuanced and accurate interpretation. When you combine its subjective data with objective findings, a complete picture of the patient's condition starts to emerge.
Here are three actionable strategies to build that complete picture:
Conduct a Thorough Clinical Interview: This is non-negotiable. Always start with a detailed conversation about the patient’s history. Ask about their pre-injury baseline, lifestyle, stress levels, and any other health conditions. This context is critical for separating concussion symptoms from everything else.
Incorporate Objective Measures: Pair the RPQ with hands-on assessments. Think balance tests, neurocognitive testing, or a vision screening. For example, if a patient reports "blurred vision" with a score of 3, an objective vision exam can confirm whether there's a real functional deficit, providing a clear path for referral to a specialist.
Track Symptoms Over Time: A single RPQ score is just a snapshot in time. Real insight comes from tracking scores longitudinally. If a patient's scores on cognitive items get better with therapy, but their emotional symptoms stay stubbornly high, that’s a huge clue that you need to explore other factors like mood or stress.
Using this kind of layered approach allows clinicians to play to the RPQ's strengths while neatly sidestepping its weaknesses. This balanced perspective ultimately leads to sharper diagnoses and treatment plans that are truly personalized and effective.
To see how modern digital platforms can help track these assessments and provide the objective cognitive data needed to complement the RPQ, visit our website to explore the solutions offered by Orange Neurosciences.
Bringing the RPQ into the Digital Age
The Rivermead Post‑Concussion Symptoms Questionnaire gives us a vital window into a patient’s subjective experience. But on its own, it's a static snapshot. By pairing it with modern digital health tools, we can transform that snapshot into a dynamic, data-rich story of recovery.
Think about this practical clinic workflow: A patient fills out the questionnaire on a tablet in the waiting room. Before they walk into your office, the scores are automatically calculated and graphed against their previous results. This simple shift frees up precious consultation time, letting clinicians focus on the patient, not the paperwork.

This digital approach does more than just save time; it creates a seamless way to track a patient’s recovery from one appointment to the next.
Building a Clearer Recovery Story
Digital platforms go far beyond simple scoring. They act as a central, secure hub for all patient data, turning isolated RPQ scores into a continuous narrative of their healing process.
This brings some massive advantages and actionable insights:
Automated Scoring: This completely removes the risk of manual calculation errors and delivers immediate results.
Secure Cloud Storage: All patient data is kept safe and organized in one place, ready to be accessed whenever needed. Of course, patient privacy is non-negotiable, which is why any platform must follow strict guidelines for HIPAA compliant app development.
Data Visualization: The best platforms can generate simple, easy-to-read graphs that chart a patient’s symptom scores over weeks or months. This makes progress—or a frustrating plateau—immediately obvious, providing a clear visual aid to use when discussing the treatment plan with the patient.
Seeing their progress mapped out visually can be incredibly powerful and motivating for patients. It gives them tangible proof that their hard work is paying off and helps them stay committed to their recovery plan.
Creating a Complete Picture of Recovery
Here’s where digital integration truly shines: it allows us to merge the subjective data from the RPQ with objective cognitive measures. A high score for "poor concentration" tells you what the patient is feeling, but an objective cognitive test can show you how that feeling is actually impacting their attention and processing speed in real-time.
By pairing the RPQ with objective cognitive assessments, clinicians can build a 360-degree view of a patient’s recovery. This combination of subjective experience and objective data leads to more precise, personalized, and effective care plans.
This is exactly where platforms like Orange Neurosciences step in. We integrate trusted tools like the Rivermead Concussion Questionnaire with our own objective cognitive assessments, helping clinicians build a truly complete profile of a patient's brain health. This unified approach takes the guesswork out of the equation and empowers genuinely data-driven decisions.
To see how this works in a real-world clinical setting, explore the details of our solution and learn how you can bring a new level of clarity to your concussion management workflow. Or email us directly to discuss your specific needs.
Frequently Asked Questions
When you’re considering a new clinical tool, questions always come up. Let’s tackle some of the most common ones about the Rivermead Concussion Questionnaire to clear things up and reinforce what we’ve covered.
How Long Does It Take to Complete?
One of the best things about the RPQ is how quick it is. Most people can get through all 16 questions in just 5 to 10 minutes.
This efficiency is a huge plus in a busy clinic. A patient can fill it out in the waiting room before their appointment, giving you valuable data without slowing down your schedule.
Can It Be Used for Children?
The RPQ was built and tested for adolescents and adults. While some clinicians might try to adapt it for younger patients, it’s not really the right tool for the job.
For pediatric cases, you’re much better off with assessments designed specifically for kids. A great alternative is the Child-SCAT, which is tailored for evaluating concussions in patients aged 12 and under.
How Often Should It Be Used During Recovery?
There's no one-size-fits-all answer here; it really depends on the patient and their recovery path.
Acute Phase: Right after the injury, you might use it weekly to keep a close eye on symptoms as they change.
Long-Term Management: For those with lingering issues, a monthly check-in can be perfect for tracking slower, more gradual improvements.
The most important thing is consistency. Using the RPQ at regular intervals helps you build a clear data story over time. An actionable insight from this data is knowing when to adjust the care plan. For example, an athlete might need weekly tracking to guide their return-to-play protocol, while an office worker might just need it at each monthly follow-up.
Is It a Standalone Diagnostic Tool?
Absolutely not, and this is a critical point. The Rivermead Concussion Questionnaire is a symptom severity scale, not a diagnostic instrument.
It tells you how much symptoms are bothering a patient, but it can’t diagnose a concussion on its own. Think of it as one important piece of a much larger puzzle, which should always include a full clinical interview and other objective tests.
Ready to see how objective cognitive data can complement the insights from the RPQ? The team at Orange Neurosciences can show you how our platform provides the deeper data you need for a complete picture of brain health. Discover more at https://orangeneurosciences.ca or email us to get started.

Orange Neurosciences' Cognitive Skills Assessments (CSA) are intended as an aid for assessing the cognitive well-being of an individual. In a clinical setting, the CSA results (when interpreted by a qualified healthcare provider) may be used as an aid in determining whether further cognitive evaluation is needed. Orange Neurosciences' brain training programs are designed to promote and encourage overall cognitive health. Orange Neurosciences does not offer any medical diagnosis or treatment of any medical disease or condition. Orange Neurosciences products may also be used for research purposes for any range of cognition-related assessments. If used for research purposes, all use of the product must comply with the appropriate human subjects' procedures as they exist within the researcher's institution and will be the researcher's responsibility. All such human subject protections shall be under the provisions of all applicable sections of the Code of Federal Regulations.
© 2025 by Orange Neurosciences Corporation



