Your Guide to the Postconcussion Symptoms Questionnaire
Oct 20, 2025
Think of a postconcussion symptoms questionnaire as a detailed map for your recovery journey. It’s a tool designed to help you and your healthcare provider translate those confusing, hard-to-describe feelings like dizziness or 'brain fog' into clear, trackable data.
This actionable data allows you to take control of your recovery, ensuring your treatment plan is perfectly tailored to what you’re experiencing right now.
Your Guide to Postconcussion Symptoms Questionnaires
After a mild traumatic brain injury (mTBI), the symptoms can feel overwhelming and frustratingly vague. A postconcussion symptoms questionnaire brings much-needed structure to the chaos by providing a checklist of common symptoms.
You’ll rate the severity of each one, which creates a consistent snapshot of how you're feeling at that moment. This isn't just a list; it’s a powerful communication tool.
For instance, instead of just telling your doctor, "I feel off," you can provide actionable insight. A practical example would be: "My headaches are a '3' (moderate) on the scale, especially after 20 minutes of screen time, while my sensitivity to light is a '4' (severe) in brightly lit stores." This tangible data makes for a much more productive conversation, ensuring no symptom gets overlooked and your treatment can be targeted effectively.
This infographic breaks down the simple but effective process of using a postconcussion symptoms questionnaire.
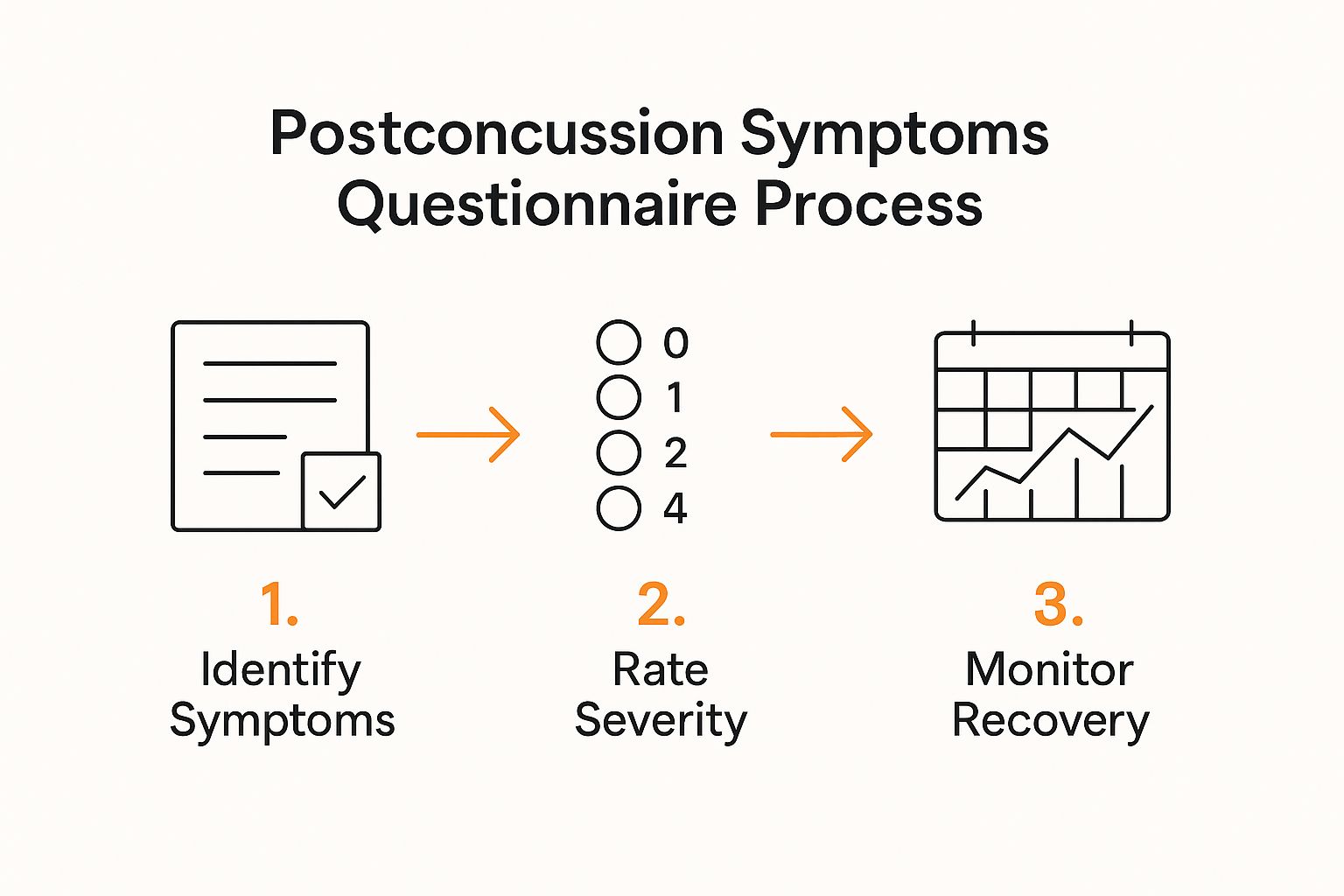
As you can see, the process flows from pinpointing your specific symptoms to rating their severity. This is what provides the essential data needed to monitor your recovery over time.
The Purpose of a Symptoms Questionnaire
At its core, the questionnaire's main job is to monitor your recovery, flag persistent issues, and help guide treatment decisions. While different versions exist, a common one used here in Canada is the Rivermead Post-Concussion Symptoms Questionnaire (RPQ).
This standardized approach offers a few key benefits:
Objective Tracking: By comparing your scores over weeks or months, you and your doctor can see a clear trend: are symptoms getting better, staying the same, or getting worse?
Targeted Treatment: If the questionnaire consistently shows high scores for dizziness, your doctor has a clear reason to suggest vestibular therapy. If cognitive issues like memory problems are flagged, it provides an actionable next step, like a referral for further evaluation. Our guide on what is a cognitive assessment offers more context on that process.
Empowered Participation: Using this tool makes you an active, informed partner in your own recovery. You’re no longer a passenger; you’re helping navigate.
A postconcussion symptoms questionnaire helps quantify the subjective experience of recovery. It turns abstract feelings into concrete data points that can guide a more effective and personalized treatment plan.
Unfortunately, a staggering number of symptoms go unreported. In Canada, 21.9% of people who sustained a concussion didn't seek medical care within 48 hours. This means many of the very symptoms these questionnaires are designed to capture are never documented. You can dig into more of this data from Statistics Canada on concussion reporting trends in Canada.
How to Use and Score the Questionnaire

Putting a post-concussion questionnaire to use is a refreshingly simple process, both for the person experiencing symptoms and the clinician guiding them. The whole point is to take those hard-to-describe feelings—the brain fog, the dizziness, the irritability—and turn them into clear, objective data. This information is invaluable for tracking recovery and making sure your treatment plan is on the right track.
Let's walk through how it's done, using a very common tool as our guide.
One of the most trusted questionnaires you'll see in Canadian clinics is the Rivermead Post-Concussion Symptoms Questionnaire (RPQ). It's a straightforward list of 16 common symptoms, and your job is to rate how much each one has been a problem over the past 24 hours. You can get a closer look at the specifics by checking out the official guidelines for the Rivermead questionnaire1.pdf).
The 5-Point Rating Scale
To keep things consistent, each symptom is rated on a simple 5-point scale, from 0 to 4. This scale is the key to turning a subjective feeling into a number that can be tracked over time.
To make this crystal clear, we've put together a table that breaks down what each score really means with practical examples.
Understanding the RPQ Scoring Scale
Score | Patient Rating | Practical Example for 'Headaches' |
|---|---|---|
0 | Not experienced at all | "I haven't had a single headache in the last 24 hours." |
1 | No problem | "I felt a slight twinge, but it passed quickly and didn't bother me." |
2 | A mild problem | "I had a noticeable but manageable headache; it didn't stop me from my usual activities." |
3 | A moderate problem | "My headache was persistent and distracting, making it hard to focus on work." |
4 | A severe problem | "The headache was debilitating. I had to stop what I was doing and rest." |
Thinking about your symptoms this way helps you give a much more accurate picture of what you're going through, moving beyond just saying "my head hurts."
Calculating Your Total Score
Once you’ve rated all 16 symptoms, getting your total score is just a matter of simple addition. You just add up the numbers you assigned to each item.
The final score can fall anywhere between 0 (meaning no symptoms at all) and 64 (meaning every symptom is severe). This one number gives you and your healthcare provider a quick, at-a-glance measure of your overall symptom load.
The total score is a powerful benchmark. By comparing your score from one week to the next, you and your healthcare provider can objectively see if your recovery is progressing, stalling, or regressing.
Understanding Sub-Scores
Digging a little deeper, the RPQ can also be broken down into two very useful sub-scores. This clever split helps distinguish between the physical symptoms that often show up right away and the cognitive or emotional ones that can linger.
RPQ-3: This is simply the total score from the first three items on the list: headaches, dizziness, and nausea/vomiting. These are often the "big three" symptoms that appear immediately after an injury.
RPQ-13: This score is the sum of the other 13 items. This group includes symptoms like irritability, forgetfulness, and fatigue—the kind of cognitive and emotional challenges that can become more apparent as the initial physical symptoms fade.
By looking at these scores separately, your clinician gets a more detailed story. For instance, a high RPQ-3 score is pretty typical in the first few days. But if the RPQ-13 score stays high weeks later, it signals that the cognitive side of things might need more targeted attention. These cognitive challenges are often explored with other specialized tools, which you can learn about in our guide to the Frontal Assessment Battery.
What Your Questionnaire Results Actually Mean

Getting a single score from your postconcussion symptoms questionnaire is really just the first step. Think of it like a single snapshot from a long road trip; it captures one moment in time, but it doesn't tell the whole story of the journey.
The real insight comes from looking at the entire photo album—tracking how your scores change over several weeks or months. This trend line is far more revealing than any single number.
A single high score, especially right after an injury, isn't necessarily a reason to panic. What truly matters is the direction that score is heading in over time.
Interpreting Trends In Your Scores
Your results are primarily measured against your own previous scores. You are your own benchmark. This personal baseline is what makes the questionnaire such a powerful, tailored tool for your recovery.
Here’s how these trends can provide actionable insight in a real-world scenario:
A Clear Sign of Progress: If your total score drops from 45 to 20 over four weeks, that's fantastic. It's measurable proof that your recovery plan is working and you can continue with the current approach.
A Signal to Re-evaluate: On the other hand, if a score stays stubbornly high—or even creeps up—over that same period, it's a red flag. This provides an actionable insight: the current strategies probably aren't cutting it and your care team needs to rethink the approach.
The most critical piece of information you can get from the questionnaire is your score's trend. A consistently decreasing score is exactly what we want to see. It’s a strong signal that your brain is healing and symptoms are resolving.
How Clinicians Use Your Results
For a clinician, these trends are gold. They allow us to make informed, data-driven decisions about your care instead of just guessing.
The questionnaire helps us zero in on specific, stubborn issues that might otherwise get lost in the shuffle. For instance, maybe your total score is improving, but your ratings for "dizziness" and "balance problems" are still high. This gives your doctor a clear, objective reason to recommend targeted physiotherapy or vestibular therapy.
It's the same for cognitive symptoms. If things like "forgetfulness" or "difficulty concentrating" aren't getting better, that's a clear signal to bring in more specialized support. This is often where exploring different cognitive therapies becomes a crucial next step, helping to retrain the brain and build new coping strategies.
Your questionnaire results empower your healthcare team to create a dynamic treatment plan that adapts to your unique recovery path. But, and this is important, these scores need a professional eye. Always work with a qualified healthcare provider who can place your results in the full context of your health and build a safe, effective recovery plan just for you.
Feel free to email our team to learn how we can help guide you through this process.
Managing Long-Term Concussion Symptoms
For most people, concussion symptoms fade away within a few weeks. But what happens when they don't? When symptoms linger for months, it's often called Persistent Post-Concussion Symptoms (PPCS), and navigating this longer, more complex recovery journey requires a different approach.
This is where a postconcussion symptoms questionnaire becomes absolutely essential.

It gives you and your healthcare team consistent, objective evidence of your ongoing struggles. That data isn't just for tracking—it's vital for validating your experience and can be crucial when you need to arrange continued care, insurance support, or accommodations at work or school.
Using The Questionnaire For Targeted Treatment
Think of the questionnaire as a diagnostic spotlight. It illuminates the specific areas where you need the most help, providing actionable insights for your healthcare team instead of just telling you to "wait and see."
Let's look at a practical example. A patient's total score on the questionnaire stops improving after six weeks. That plateau is a clear signal to their doctor that something needs to change. By breaking down the sub-scores, they can pinpoint the exact problem:
High Physical Scores: If ratings for dizziness and balance are still elevated, it's a strong indicator that a referral to a physiotherapist who specializes in vestibular therapy is the right next move.
High Cognitive Scores: Persistent high scores for "brain fog" or memory problems might trigger a referral to a neuropsychologist for a more detailed cognitive workup.
High Emotional Scores: If irritability or anxiety scores aren't coming down, it might mean it's time to bring in a counsellor or other therapeutic support.
By highlighting these specific symptom clusters, the questionnaire allows treatment to shift from a general "rest and recover" approach to a highly personalized one. For anyone navigating the complexities of long-term concussion recovery, understanding broader funding avenues like healthcare grants can also be a game-changer, providing critical support for these specialized treatments.
A postconcussion symptoms questionnaire transforms a long-term recovery process from a waiting game into an active, data-driven strategy. It ensures that persistent symptoms are not just endured, but are actively identified and addressed.
One of the biggest challenges with PPCS is that it’s notoriously hard to predict. In fact, research shows that emergency physicians’ accuracy in forecasting who will recover at three months post-injury is no better than chance. This really underscores the limitations of relying on clinical judgment alone and reinforces the value of using a postconcussion symptoms questionnaire for consistent, ongoing monitoring.
This is especially true for tricky symptoms like sleep disturbances, which can throw a major wrench in the entire recovery process. Poor sleep often makes headaches, fatigue, and cognitive issues worse, creating a vicious cycle. If your questionnaire consistently flags sleep as an issue, it’s a clear sign that it needs to be addressed directly. You can learn more about this connection in our detailed guide on concussions and sleep.
Our team at Orange Neurosciences can help you make sense of these nuanced results. Email us to learn how we create personalized recovery plans based on your unique symptom profile.
Clearing Up Common Myths and Misunderstandings
To really get the most out of a postconcussion symptoms questionnaire, it’s important to have a clear picture of what it can and can't do. While these questionnaires are incredibly helpful, they aren't a crystal ball. Understanding their limits helps everyone—patients and clinicians alike—set realistic expectations for the recovery journey.
The biggest thing to remember is that these questionnaires are subjective. They are built entirely on how you feel and what you report. This means the results can be swayed by things that have nothing to do with a brain injury, like stress from work, a bad night's sleep, or even conditions you already had, such as anxiety or migraines.
It's a Guide, Not a Diagnosis
Here's one of the most critical takeaways: a postconcussion symptoms questionnaire is a tool for monitoring, not for diagnosis. It’s brilliant at tracking the what and how much—the presence and severity of your symptoms—but it can't tell you why they're happening.
Let's bust a common myth right now: a high score does not automatically mean you have a severe brain injury. Many of the symptoms on the list, like headaches, fatigue, or trouble concentrating, are very general. They can pop up for all sorts of reasons, which is why context is everything.
Think of the questionnaire as just one piece of your larger healthcare puzzle. It tells your doctor what you're experiencing, but it takes a trained professional to figure out the why.
This is precisely why the questionnaire should always be part of a full clinical evaluation. A healthcare professional uses it as a starting point, combining it with other tests and their own expertise to see the whole, accurate picture of your health.
Why Clinical Context Is Everything
Imagine two people fill out the same questionnaire and get identical high scores. One person was in a car accident and took a direct blow to the head. The other hasn't had any head injury but has been dealing with months of chronic stress and sleepless nights. The scores might look the same on paper, but the stories behind them are worlds apart.
A healthcare provider uses this crucial context to:
Rule out other causes: They can dig deeper to see if your fatigue is truly from the concussion or if another underlying issue is at play.
Interpret changes over time: A sudden spike in your symptom score might be a red flag for overexertion, something the questionnaire alone would never show.
Create a plan that actually works: Context ensures your treatment targets the real root of your symptoms, not just the symptoms themselves.
At the end of the day, the best way to look at the postconcussion symptoms questionnaire is as a collaborative tool. It gives you a structured way to share your experience, which in turn gives your doctor the detailed insights they need to guide your recovery effectively.
To see what this looks like in practice, we invite you to download a sample questionnaire on our website. Getting familiar with the format can help you have more productive and focused conversations with your healthcare team.
Take an Active Role in Your Concussion Recovery
This guide has walked you through how the postconcussion symptoms questionnaire puts you in the driver's seat of your own healing process. It's a powerful tool that shifts you from being a passive patient to an essential player on your recovery team.
By translating your subjective feelings into real, measurable data, the questionnaire opens the door to clearer, more productive conversations with your doctor. It allows you to track your progress objectively and helps shape a personalized treatment plan that truly adapts to your unique needs as they change over time. Now, it's time to put this knowledge to work.
Chart Your Path Forward
Navigating concussion recovery can feel isolating, but it doesn't have to be. With the right tools and support, you can absolutely take control of your journey. The data from a postconcussion symptoms questionnaire is like a map, showing you exactly where you are and where you need to go next.
This structured information is priceless, especially when you're building a complete recovery strategy. For instance, if your scores consistently flag issues with balance or cognitive fog, that's a clear signal you need specific interventions. These targeted approaches are the bedrock of effective neurorehabilitation, helping you rebuild skills and get your confidence back.
Your active involvement, guided by objective tools like the postconcussion symptoms questionnaire, is the single most important factor in a successful recovery. It ensures your treatment plan is not generic but tailored specifically to you.
You don't have to figure this out alone. We invite you to connect with our team of healthcare professionals who specialize in concussion management. Let us help you use tools like these to build a structured recovery plan that addresses your specific symptoms and gets you back on track to feeling like yourself again. Email our team today to learn more.
Still Have Questions? We've Got Answers
Working through the details of a postconcussion questionnaire can often bring up a few specific questions. Here are some quick, straightforward answers to the queries we hear most often from individuals and their families.
How Often Should I Be Filling This Out?
The honest answer? It really depends on where you are in your recovery and what your doctor recommends.
Right after an injury, it’s common to fill out the questionnaire weekly. This gives your care team a detailed, week-by-week snapshot of how things are progressing. As your symptoms start to ease up and you feel more like yourself, your doctor will likely scale it back to every two weeks, or even monthly, just to keep an eye on your long-term stability. The idea is to track the trends without adding any extra stress to your plate.
Can I Use This Questionnaire for My Child’s Concussion?
While the goal of tracking symptoms is the same for everyone, it's crucial to use a tool that’s been designed specifically for kids. A standard postconcussion questionnaire is built and tested for adults.
For children and teens, your healthcare provider will almost always use a pediatric-specific version. A great example is the Post-Concussion Symptom Inventory (PCSI). It’s tailored to how children actually experience and describe their symptoms, which leads to a much more accurate picture of what’s going on.
Your first call should always be to a paediatrician or a specialist in paediatric concussions. They have the right tools for the job and can interpret the results in the context of a developing brain—something that is absolutely critical for a safe and complete recovery.
What if My Symptoms Get Worse After They Were Getting Better?
If you notice your scores on the questionnaire starting to creep up after a period of improvement, get in touch with your doctor right away. This isn't a "wait and see" situation.
A step back in your scores could mean you’ve pushed yourself a bit too hard, too soon. A practical example is returning to a full day of work and noticing your headache score jump from a '1' to a '3'. This data gives your doctor an actionable insight: you may need to adjust your return-to-work plan with shorter days or more frequent breaks.
At Orange Neurosciences, we know that objective data is the cornerstone of a successful recovery. Our tools are designed to provide clear cognitive profiles that help clinicians build more informed and effective care plans. To see how our platform can support your journey, visit us at https://orangeneurosciences.ca.

Orange Neurosciences' Cognitive Skills Assessments (CSA) are intended as an aid for assessing the cognitive well-being of an individual. In a clinical setting, the CSA results (when interpreted by a qualified healthcare provider) may be used as an aid in determining whether further cognitive evaluation is needed. Orange Neurosciences' brain training programs are designed to promote and encourage overall cognitive health. Orange Neurosciences does not offer any medical diagnosis or treatment of any medical disease or condition. Orange Neurosciences products may also be used for research purposes for any range of cognition-related assessments. If used for research purposes, all use of the product must comply with the appropriate human subjects' procedures as they exist within the researcher's institution and will be the researcher's responsibility. All such human subject protections shall be under the provisions of all applicable sections of the Code of Federal Regulations.
© 2025 by Orange Neurosciences Corporation



