A Practical Guide to the Perceived Stress Scale
Jan 3, 2026
When you hear "stress test," you might think of a heart monitor or a physical exam. But the Perceived Stress Scale (PSS) is different. It's a psychological tool designed to measure something far more personal: the degree to which you feel the situations in your life are stressful.
Instead of just counting up difficult events, the PSS digs into your subjective experience and perceptions over the past month. This makes it an incredibly powerful gauge of your internal emotional climate, providing actionable insights you can use to improve your well-being.
Your Personal Stress Weather Report
Think of the Perceived Stress Scale less like a rigid medical test and more like a personal weather report for your mind. It doesn't just tally how many "storms" (stressful events) you've recently faced.
Instead, it measures the atmospheric pressure building inside your head—how unpredictable, uncontrollable, and overloaded you've been feeling. This distinction is crucial. Decades of research show that our appraisal of a situation, not the event itself, is what truly drives our stress levels.
For instance, two colleagues could face the exact same tight project deadline.
Person A (Low Perceived Stress): Sees it as an exciting, manageable challenge. They might think, "This is tough, but I have the skills to get it done."
Person B (High Perceived Stress): Views it as an overwhelming, uncontrollable threat. Their thought might be, "There's no way I can finish this; I'm going to fail."
The PSS is built to capture Person B's experience, translating their internal state of distress into a clear, understandable score that can guide action.
What the Perceived Stress Scale Actually Measures
At its core, the scale operates on the principle that stress is all about perception. It gets to the heart of this by asking questions that probe three key feelings:
Unpredictability: How often have you been caught off guard and upset by something unexpected? (e.g., a surprise bill, a sudden change in plans)
Lack of Control: How often have you felt you couldn't manage the important things in your life? (e.g., juggling work deadlines and family needs)
Overload: How often have you felt that your difficulties were piling up too high to overcome? (e.g., feeling like you're constantly behind on everything)
By zeroing in on these subjective feelings, the PSS provides clinicians, researchers, and individuals with a tangible measure for an experience that can often feel vague. To see exactly how these questions are framed, you can check out our detailed guide to the perceived stress questionnaire.
The Different Versions of the PSS
The PSS isn't a one-size-fits-all tool. To suit different needs, whether it's a quick clinical check-in or a deep-dive research study, it comes in a few different lengths.
Here’s a quick look at what the most common version, the PSS-10, looks like when administered digitally.
As you can see, the clean layout and simple 0-4 rating scale make the assessment quick and straightforward for users to complete.
To help you understand the options, here’s a quick summary of the most common versions of the PSS.
Perceived Stress Scale Versions at a Glance
Version | Number of Items | Primary Use Case |
|---|---|---|
PSS-10 | 10 questions | The most widely used version. Offers a great balance of speed and detail for most clinical and personal uses. |
PSS-14 | 14 questions | The original scale. Provides more nuance and is often preferred in research settings for a more granular view. |
PSS-4 | 4 questions | An ultra-brief version, perfect for large-scale surveys or quick screenings where time is extremely limited. |
Each version has its place, but they all share the same goal: to provide a reliable snapshot of your perceived stress.
Understanding this personal stress level is a vital first step toward improving mental wellness and boosting cognitive performance. At Orange Neurosciences, we integrate subjective measures like the PSS with objective cognitive data to build a complete, holistic picture of brain health.
How to Use and Score the PSS-10
Knowing you feel stressed is one thing, but actually measuring it is something else entirely. This is where the Perceived Stress Scale, especially the popular 10-item version (PSS-10), comes in. It gives us a structured way to put a number to those subjective feelings.
The process itself is pretty simple, but understanding the details of scoring is what really unlocks its value and leads to actionable insights.
When taking the PSS-10, a person reflects on their feelings and thoughts over the last month. Each of the ten questions is then rated on a 5-point scale:
0 = Never
1 = Almost Never
2 = Sometimes
3 = Fairly Often
4 = Very Often
This simple flow chart really gets to the heart of what the PSS measures. It's not the situation itself, but how we appraise—or think about—that situation that determines our stress level.
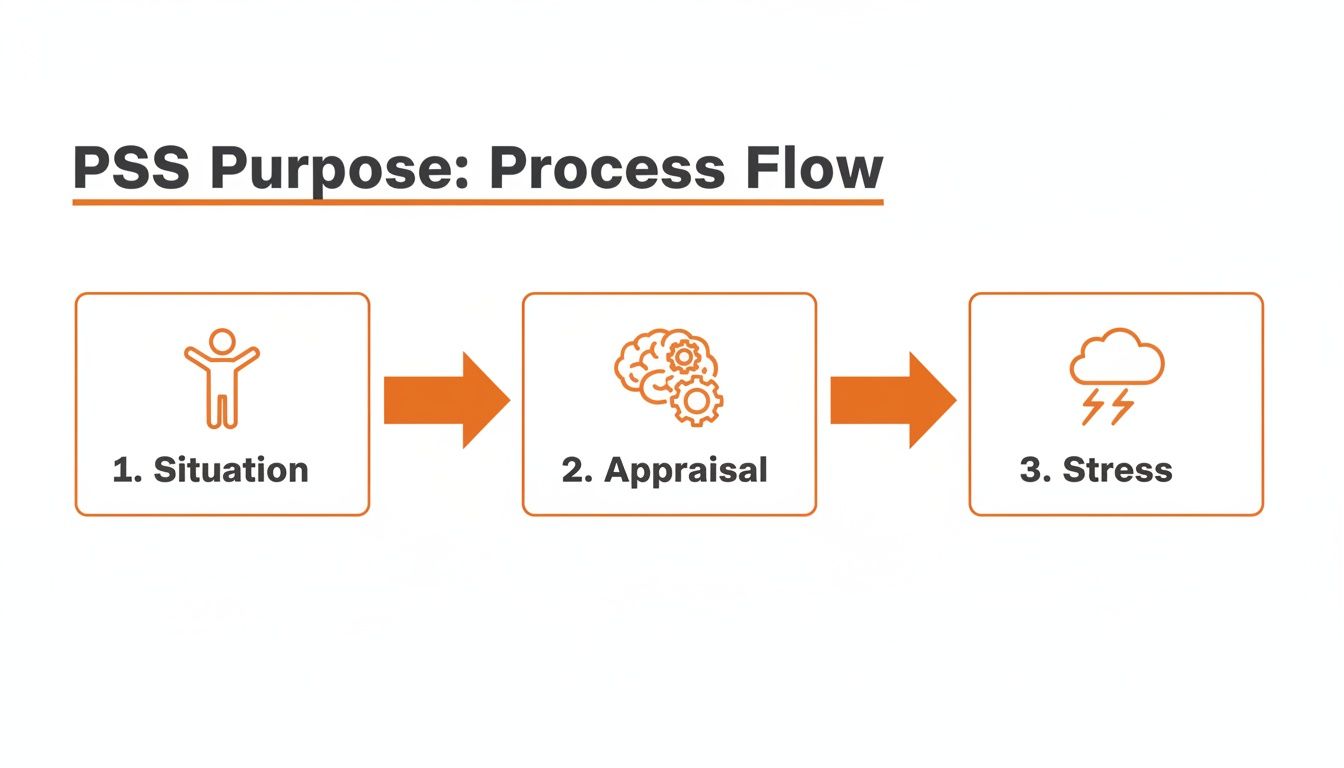
As the diagram shows, that "appraisal" step is the critical filter. It’s the personal interpretation of an event, not the event itself, that drives the stress response.
The Crucial Step of Reverse Scoring
One of the most common hangups when scoring the PSS-10 is the idea of reverse scoring. Not every question is framed negatively. Four of the items—questions 4, 5, 7, and 8—are phrased positively to measure feelings of confidence and control.
Think of these questions as gauging resilience. For instance, question 5 asks, "In the last month, how often have you felt that things were going your way?" A high score on this item actually points to low stress, so we need to flip the value.
Actionable Step: To reverse-score these positive items (4, 5, 7, 8), simply subtract the respondent's score from 4. If someone answers "Very Often" (a score of 4) on a positive question, its contribution to the final stress score becomes 0 (because 4 – 4 = 0).
Here's how it works in practice:
Original Score: A person scores a 3 ("Fairly Often") on question 7: "In the last month, how often have you felt you were able to control irritations in your life?"
Reverse Score Calculation: You take the highest possible score (4) and subtract their answer: 4 – 3 = 1.
Final Value: The new value for this item is 1. This is the number you'll use when you add everything up.
Calculating and Interpreting Your Total Score
Once you’ve reversed the scores for items 4, 5, 7, and 8, the final step is easy: just add up the values for all ten questions. Your total score will be somewhere between 0 and 40, with higher scores meaning greater perceived stress.
Generally, these totals are grouped into three levels, which gives you a handy benchmark for actionable next steps:
Low Stress (0–13): Your coping strategies are likely effective. Action: Acknowledge what's working and continue to build on those healthy habits.
Moderate Stress (14–26): This is the most common range. Action: This is a signal to proactively build better stress management habits. You might explore mindfulness, exercise, or time management techniques.
High Stress (27–40): A score this high indicates significant feelings of overwhelm. Action: This is a clear call to seek support. Consider discussing this with a healthcare professional or therapist to develop a plan.
It's important to remember these scores aren't a diagnosis; they're a powerful indicator. For clinicians, a high PSS score might be the trigger for a deeper dive. It could prompt a more comprehensive evaluation, which you can learn about in our guide on what is neuropsychological assessment.
Why Clinicians Trust the Perceived Stress Scale
For any assessment to be worth its salt in a professional setting, it needs more than just good questions. It has to be dependable and actually measure what it says it’s measuring. The Perceived Stress Scale isn't just popular because it's quick and easy; clinicians and researchers trust it because it has consistently proven to be scientifically solid. In the field, we call this having strong psychometric properties.
This rock-solid reliability is why the PSS is a cornerstone in everything from routine mental health check-ups to massive research studies. But what does that really mean in practice? It all comes down to two key ideas: internal consistency and validity.
Measuring One Thing Consistently
First off, the PSS has excellent internal consistency. This means all its questions are working in harmony to measure a single, unified concept: your personal, subjective feeling of stress.
Think of it like a well-designed symphony. Each question on the PSS tackles perceived stress from a slightly different angle, but together, they produce a single, reliable score that truly reflects a person's internal state.
This consistency is crucial. It gives clinicians the confidence that the score isn't just a random assortment of answers, but a meaningful measurement of the psychological pressure someone is under.
This principle holds up even when the scale is adapted for different groups. For example, a validation study of 450 early childhood teacher candidates found that a staggering 52% reported high distress. Their average score was 51% higher than general population norms—a clear reflection of the immense strain from recent teacher shortages. Even with cultural and language adjustments, the scale’s internal consistency was strong, proving it’s a reliable tool. You can dive into the specifics of the validation study on early childhood educators.
Accurately Predicting Real-World Outcomes
Beyond just being consistent, the Perceived Stress Scale also shows strong construct validity. Put simply, this means PSS scores connect in a meaningful way to real-world health outcomes. Study after study shows that higher PSS scores are strongly correlated with higher levels of anxiety and depression.
Let’s look at a practical, actionable example:
A patient, Alex, mentions feeling "on edge" during a routine check-up. His doctor has him complete the PSS-10, and Alex scores a 28 (high stress).
Because of the scale's predictive power, the doctor knows this score is a red flag. It’s the catalyst for a deeper conversation about Alex's mood and anxiety levels.
The Actionable Insight: The high score prompts the doctor to screen for anxiety. This leads to a more thorough evaluation, revealing an anxiety disorder that might have otherwise been missed.
This predictive ability is what elevates the PSS from a simple questionnaire to a proactive screening tool. By giving us a reliable window into a person’s internal world, it helps professionals spot risks and intervene much earlier. Tools like these are often covered in our detailed clinical knowledge summaries, which explore how different assessments can guide better care.
Practical Applications in Healthcare and Research
So, how does the Perceived Stress Scale move from a theoretical concept to something that makes a real-world difference? Its true power isn't just in its scientific validation but in how practical and actionable it is for professionals on the ground.
For healthcare providers, it’s a remarkably efficient way to screen patients and flag those at risk for stress-related problems. It provides a simple, structured way to start a conversation about mental well-being.

Practical Example: A family doctor gives a patient the PSS-10 during a routine annual check-up. The patient scores a 31. This high score is the first clue that chronic stress might be contributing to their high blood pressure.
Actionable Step: Instead of just refilling a prescription, the doctor can now say, "Your stress score is quite high. Let's talk about what's going on and explore some stress management strategies that could also help your blood pressure."
This simple step shifts the focus from just treating symptoms to preventing bigger problems down the road.
A Tool for Tracking Progress and Adjusting Care
The PSS is also incredibly valuable in rehabilitation settings, where it helps track a patient's psychological journey right alongside their physical recovery.
Practical Example: A physiotherapist working with someone recovering from a car accident uses the PSS monthly. They notice the patient's score has jumped from 15 to 25.
Actionable Step: This rising score is an early warning sign that the patient is feeling overwhelmed. The therapist can now adjust the care plan, perhaps by integrating mindfulness exercises or referring the patient to a counsellor, ensuring a more holistic recovery.
This ongoing monitoring provides clear, objective data to guide what can often be very subjective care decisions.
Informing Vital Interventions in High-Stress Environments
In the world of research, the PSS is a powerful instrument for digging into the complex links between stress, behaviour, and health.
One California study of over 1,200 healthcare workers during the COVID-19 pandemic used the PSS-10 to capture the intense pressure they were under. The results were stark: 68% scored in the moderate to high stress range. Emergency room nurses reported an average score of 25.4—nearly double the national baseline.
This data wasn't just a number; it correlated strongly with burnout, with 42% meeting the criteria for clinical burnout.
Actionable Outcome: This hard evidence was used to advocate for real, systemic changes, such as targeted mental health support programs for high-risk roles, adjustments to staffing levels, and resilience training to equip staff with better coping mechanisms.
Once perceived stress is identified, the next step is knowing what to do with that information. For instance, you can explore insights into recognizing signs of stress in children and how to support students. By translating subjective feelings into objective data, the scale empowers professionals to make better-informed decisions that genuinely improve lives.
Pairing the PSS with Digital Cognitive Assessments
The Perceived Stress Scale gives us a crucial piece of the puzzle: a person's subjective feeling of being overwhelmed. But what happens when we pair that feeling with hard, objective data about how their brain is actually performing? This is where the true power of an integrated approach comes to light, transforming a general feeling of "I'm stressed" into a specific, actionable diagnostic roadmap.
Combining the PSS with modern digital cognitive assessments creates a much richer, more complete picture of an individual's brain health.
From Subjective Feeling to Objective Deficits
High levels of chronic stress aren't just an emotional burden; they have a real, physical impact on the brain. When someone scores high on the PSS, it's often a strong indicator that certain cognitive functions may be struggling. Platforms like Orange Neurosciences are designed to precisely measure these functions.
Key areas often affected by stress include:
Attention: Difficulty concentrating or staying focused.
Processing Speed: Taking longer to think and react.
Executive Function: Struggling with planning and problem-solving.
By using digital tools to assess these areas, a clinician can see the tangible effects of stress. A high PSS score is no longer just a feeling; it's linked to concrete data points. You can explore more about how these evaluations work in our overview of cognitive assessments.
A Practical Example of Integrated Data
Let's walk through a practical scenario. A patient named Mark completes the PSS-10 and scores a 29, pointing to high perceived stress. He reports feeling constantly overloaded.
On its own, this score is a valuable red flag. But when his clinician pairs it with a digital assessment like OrangeCheck, they discover more. The assessment reveals that Mark’s processing speed is significantly slower than age-appropriate norms.
Actionable Insight: The clinician can now connect the 'what' with the 'why'. The 'what' is that Mark feels overwhelmed (his high PSS score). The 'why' is that his slow processing speed is making everyday tasks more difficult, contributing to his sense of overload. This moves the conversation from a general discussion about "managing stress" to a targeted plan to address specific cognitive weaknesses.
Creating More Targeted and Effective Interventions
This combination of subjective and objective data is where treatment becomes truly personalized.
For Mark, this might mean a care plan that includes personalized, game-based training designed to improve his processing speed. As he engages with these exercises, his clinician can track his cognitive improvements objectively while also using the PSS to monitor his subjective feelings of stress.
Research supports this powerful link. A longitudinal analysis tracked 850 adults and found that seniors with mild cognitive impairment had PSS scores 62% higher than their healthy peers. Clinicians using platforms like Orange Neurosciences have also observed that patients with high PSS scores often show 25% slower processing speeds.
The positive outcome is clear: therapists have reported a 29% improvement in PSS scores after just eight weeks of targeted, game-based training. You can read the full research about these findings to see the data in detail.
For individuals looking to explore digital tools that can complement the insights gained from the PSS, a variety of resources exist, including some of the best free anxiety apps.
Limitations and Important Considerations
The Perceived Stress Scale is a fantastic tool, but like any instrument, you have to know its limits to use it well. The biggest thing to remember is that it’s subjective. The results are a direct reflection of how someone is feeling, which can be swayed by their mood that day or how they interpret the questions.
A Snapshot, Not a Feature Film
It's also crucial to see the PSS for what it is: a snapshot in time. The scale is built to capture feelings over the past month. That’s great for seeing how things are going right now, but it’s not a lifelong diagnosis.
Actionable Insight: Think of the Perceived Stress Scale as a highly effective screening tool, not a standalone diagnostic instrument. A high score is a signal to investigate further, not a final conclusion.
Cultural Context Is Key
How we define and experience stress isn't universal; it can vary wildly across different cultures. What one culture sees as a normal, everyday challenge, another might find incredibly stressful. This means we have to use the scale with sensitivity and awareness.
At the end of the day, the sharpest and most useful insights come from using the PSS as one piece of a much larger puzzle. When you pair a subjective measure like the perceived stress scale with clinical interviews and objective data—like the precise cognitive metrics you get from platforms like Orange Neurosciences—you start to see the whole person, not just a single score.
Your Questions About the PSS, Answered
As you get ready to use the Perceived Stress Scale, a few common questions are bound to pop up. Let's tackle them head-on so you can use this tool with confidence.
Can I Use the Perceived Stress Scale on Myself?
Absolutely. The PSS is a fantastic tool for self-assessment. It offers a structured way to check in with yourself and put a number to those feelings of stress.
But a high score is like a warning light on your dashboard—it tells you that you're feeling overwhelmed. A trained professional, however, can look under the hood to understand why that light is on.
Actionable Step: If you score in the moderate or high range, consider it your cue to open a conversation with a doctor or therapist. Share your score with them as a starting point.
How Often Should I Take the PSS?
The PSS is designed to capture your feelings over the previous month, which makes it perfect for tracking changes over time. Taking it monthly or every other month is usually the sweet spot.
Practical Example: A therapist might have a client take the PSS at the start of treatment and then again every four weeks. This creates a clear, objective way to see if stress management strategies are actually working and allows them to adjust the care plan as needed.
Is the PSS a Good Fit for Children and Teenagers?
The standard PSS is generally considered appropriate for anyone aged 12 and up. For younger kids, though, some of the concepts can be a bit too abstract. Trying to explain "uncontrollable" to an eight-year-old can be tricky.
Actionable Advice: For younger children, it's better to use assessment tools designed specifically for them. These scales use more concrete language and scenarios a child can relate to, ensuring you get more accurate and meaningful results.
Ready to move from subjective feelings to objective data? Orange Neurosciences combines self-reported measures like the PSS with precise, digital cognitive assessments to create a complete picture of brain health. Discover how our platform can help you make faster, better-informed decisions. Explore our solutions at https://orangeneurosciences.ca or contact us today to learn more.

Orange Neurosciences' Cognitive Skills Assessments (CSA) are intended as an aid for assessing the cognitive well-being of an individual. In a clinical setting, the CSA results (when interpreted by a qualified healthcare provider) may be used as an aid in determining whether further cognitive evaluation is needed. Orange Neurosciences' brain training programs are designed to promote and encourage overall cognitive health. Orange Neurosciences does not offer any medical diagnosis or treatment of any medical disease or condition. Orange Neurosciences products may also be used for research purposes for any range of cognition-related assessments. If used for research purposes, all use of the product must comply with the appropriate human subjects' procedures as they exist within the researcher's institution and will be the researcher's responsibility. All such human subject protections shall be under the provisions of all applicable sections of the Code of Federal Regulations.
© 2025 by Orange Neurosciences Corporation



