A Clinician's Guide to Mental State Assessment
Dec 22, 2025
A mental state assessment is, quite simply, a structured snapshot of a person's psychological functioning at a specific moment. Think of it as a systematic 'weather report' for the mind—it helps clinicians get a clear picture of an individual's current thinking, feeling, and behaviour. This process is just as fundamental to mental healthcare as a physical exam is to general medicine, providing actionable insights from the very first interaction.
Understanding The Foundations Of Mental State Assessment

A mental state assessment isn't just a rigid checklist or a formal test. It’s a dynamic blend of careful observation and guided conversation, designed to capture the "here and now." By gathering this essential information, clinicians can begin to formulate a diagnosis, map out a treatment plan, and track a person's progress over time.
This initial snapshot provides a crucial baseline. Down the road, it can be referenced to see if a patient’s condition is improving, worsening, or holding steady. It’s truly a cornerstone of clinical practice, offering a structured framework for making sense of an individual's psychological well-being.
Why This Assessment Matters
The importance of a reliable mental state assessment really can't be overstated, especially as mental health challenges continue to rise across the globe. Part of understanding these assessments involves defining the conditions they help identify, like learning What Is Substance Use Disorder.
The need is particularly stark in certain regions. For instance, mental health issues in the Caribbean are intensifying, with anxiety disorders affecting 7.3% of the population in Latin America and the Caribbean in 2021. That figure is significantly higher than both the OECD countries (6.4%) and the global average (4.7%). As detailed in a UNDP analysis of mental health in the region, this represents a sharp increase from around 5.5% two decades ago—a widening gap fuelled by economic instability and post-pandemic stress that demands robust assessment protocols.
Key Goals Of The Assessment
Ultimately, a mental state assessment is about answering several critical questions that guide the entire care pathway.
Establishing a Baseline: It creates a detailed snapshot of a person’s mental state at the very first point of contact.
Informing Diagnosis: Observations from the assessment provide crucial data to support or rule out specific mental health conditions.
Guiding Treatment: The findings help clinicians tailor interventions that address the most pressing symptoms and challenges.
Monitoring Change: It allows for tracking changes over time—an essential step for seeing if a treatment plan is actually working.
A mental state assessment provides the essential framework for organising clinical observations. It transforms subjective experiences into structured data, making it possible to develop a clear, actionable picture of a person's psychological health.
While this assessment focuses on the immediate clinical picture, it often serves as a stepping stone to more detailed testing. For those who need a deeper dive into the relationship between brain and behaviour, it’s also helpful to understand what is neuropsychological assessment and how it differs. Think of this initial evaluation as the first, foundational step in a comprehensive care journey.
Decoding the Core Domains of an Assessment
Think of a mental state assessment like a skilled mechanic diagnosing a car. They don't just look at the outside; they check the engine, the transmission, and the electrical systems individually to understand how the whole vehicle is running. Similarly, clinicians examine distinct areas of psychological functioning to build a detailed, layered picture of a person's current condition.
Let's break down what these core domains are and what they actually look like in practice. The process usually starts with the most obvious information—what you can see and hear—which lays the groundwork for the deeper, more conversational parts of the assessment.
Appearance and Behaviour
This is all about what you can see. It involves observing a person’s physical presentation and their actions, which can offer important—though not definitive—clues about what’s going on inside.
Appearance: This includes things like hygiene, grooming, and whether their clothing makes sense for the weather. For example, a client with severe depression might present with unkempt hair and disheveled clothes, while someone wearing a heavy winter coat in the middle of a July heatwave might be experiencing disorganized thinking.
Behaviour: Clinicians also pay close attention to posture, facial expressions, and motor activity. Are they constantly fidgeting and wringing their hands? That could point to significant anxiety. Or are they slumped over with very little movement? That might be a sign of depression. Even eye contact—whether it's steady, fleeting, or avoided altogether—is a key piece of the puzzle.
Mood and Affect
Most people use "mood" and "affect" interchangeably, but in a clinical setting, they mean two very different things. Getting the distinction right is crucial for an accurate assessment.
Here's a helpful way to think about it: mood is the overall climate of a person’s emotional world, their long-term, internal feeling state. In contrast, affect is the daily weather—the observable, moment-to-moment expression of their feelings.
A person might tell you their mood is "depressed" (the climate), but their affect could be tearful one moment and completely flat or unresponsive the next (the changing weather). A key part of the assessment is noticing if their expressed feelings match their internal state.
Thought Process and Content
This domain is where a clinician tries to understand how a person thinks (their process) and what they are thinking about (their content). It’s a window into the organisation and substance of their inner world.
Thought Process is all about the flow and connection of ideas. Is their speech coherent and easy to follow, moving logically from one point to the next? Or do they jump between unrelated topics (flight of ideas) or get sidetracked by irrelevant details (circumstantiality)?
Thought Content zeroes in on the specific themes that are present. This means looking for things like:
Obsessions: Persistent, intrusive thoughts or ideas they can't shake.
Delusions: Fixed, false beliefs that hold firm even when faced with contrary evidence.
Suicidal or Homicidal Ideation: Any thoughts related to harming themselves or others.
For example, a patient with a logical thought process might still have distressing thought content. They might say, "I know I shouldn't worry, but I can't stop thinking that I left the oven on," which suggests an obsession. This tells the clinician that while the mechanics of their thinking are fine, the focus of their thoughts is the source of major distress.
Cognition, Insight, and Judgment
The final core domains look at higher-level mental functions. This is where we get a sense of a person's self-awareness and their ability to make decisions.
Cognition is a broad category covering mental processes like attention, memory, and orientation. A clinician might ask simple questions like, "Who is the current Prime Minister?" or test short-term memory by asking the person to recall three objects after a few minutes. Significant struggles with cognition can sometimes point to underlying neurological issues. You can learn more about how to formally test for executive dysfunction in more specialized evaluations.
Insight is about a person's awareness of their own situation. Do they understand that their experiences—like hearing voices—are symptoms of an illness, or do they believe those experiences are completely real? Someone with poor insight is less likely to see the need for treatment.
Judgment assesses a person's ability to make sound decisions in their life. A clinician might pose a hypothetical, like "What would you do if you found a stamped, addressed envelope on the street?" to get a feel for their problem-solving skills and grasp of social norms. Poor judgment often shows up in a pattern of recent life choices that have led to negative outcomes.
Choosing the Right Assessment Tools
Once you have a handle on the foundational domains of a mental state assessment, the next step is translating those qualitative observations into something more concrete. This is where specific assessment instruments come into play, acting like specialized lenses that bring different aspects of mental functioning into sharp focus.
But here’s the thing: these tools are not one-size-fits-all. Choosing the right one is a critical clinical decision that hinges entirely on the context—the "why" behind the assessment. They range from quick, targeted screeners to much more detailed instruments for a deep cognitive dive. The key is to match the tool to the clinical setting and the patient's presenting concerns, ensuring the data you gather is both relevant and actionable.
Brief Screeners for Targeted Concerns
Think of brief screening tools as the clinical equivalent of a quick temperature check. They're designed to be fast, easy to administer, and focused on flagging potential signs of common conditions like depression or anxiety. Their primary job isn’t to diagnose, but to signal that a more thorough evaluation might be needed.
A perfect practical example is the Patient Health Questionnaire-9 (PHQ-9). A family doctor can use this nine-question tool during a routine check-up to quickly gauge the severity of depressive symptoms. Actionable insight: A score above 10 often triggers a direct conversation about mental health support or a referral to a therapist, turning a routine visit into a proactive intervention.
Similarly, the Generalised Anxiety Disorder-7 (GAD-7) does the same for anxiety. These screeners give you a simple, numerical score that helps quantify a patient's experience, making it much easier to track symptoms over time.
Comprehensive Instruments for Deeper Evaluation
When a simple screening won't cut it, clinicians turn to more comprehensive instruments. These tools offer a much more detailed and wide-ranging look at a person's cognitive or overall mental state. They’re less like a quick temperature check and more like a full diagnostic scan, providing a richer, more nuanced picture.
The Mini-Mental State Examination (MMSE) and the Montreal Cognitive Assessment (MoCA) are two of the heavy hitters in this category. You’ll often see them used when there are concerns about cognitive decline, such as potential dementia or impairment following a brain injury.
These assessments dig into multiple cognitive domains, including:
Orientation: Knowing the date, where they are, etc.
Memory: Both immediate recall and short-term memory.
Attention: The ability to focus and perform simple calculations.
Language: Naming objects, following commands, and writing.
The MoCA, in particular, is valued for its sensitivity in detecting mild cognitive impairment. For clinicians wanting to use it effectively, it's a good idea to review detailed guidance on the Montreal Cognitive Assessment instructions to ensure administration is standardized and accurate.
Deciding between a quick screener and a comprehensive tool really comes down to what you need to know. The table below breaks down the key differences to help guide that choice.
Screening Tools vs Comprehensive Assessments
Feature | Brief Screening Tools (e.g., PHQ-9, GAD-7) | Comprehensive Instruments (e.g., MMSE, MoCA) |
|---|---|---|
Purpose | Rapidly identify at-risk individuals | Provide a detailed cognitive profile |
Setting | Primary care, general check-ups | Specialty clinics, neurology, geriatrics |
Time | 5-10 minutes | 15-30 minutes or longer |
Focus | Specific conditions (e.g., depression, anxiety) | Multiple cognitive domains (memory, attention, language) |
Outcome | A score indicating risk or symptom severity | A detailed profile of cognitive strengths and weaknesses |
Next Steps | Triggers referral for further evaluation | Informs diagnosis and detailed treatment planning |
Ultimately, brief screeners tell you if there might be a problem, while comprehensive instruments help you understand what and how severe that problem is.
This flowchart illustrates how a clinician might start assessing thought organization just by observing a patient's speech.
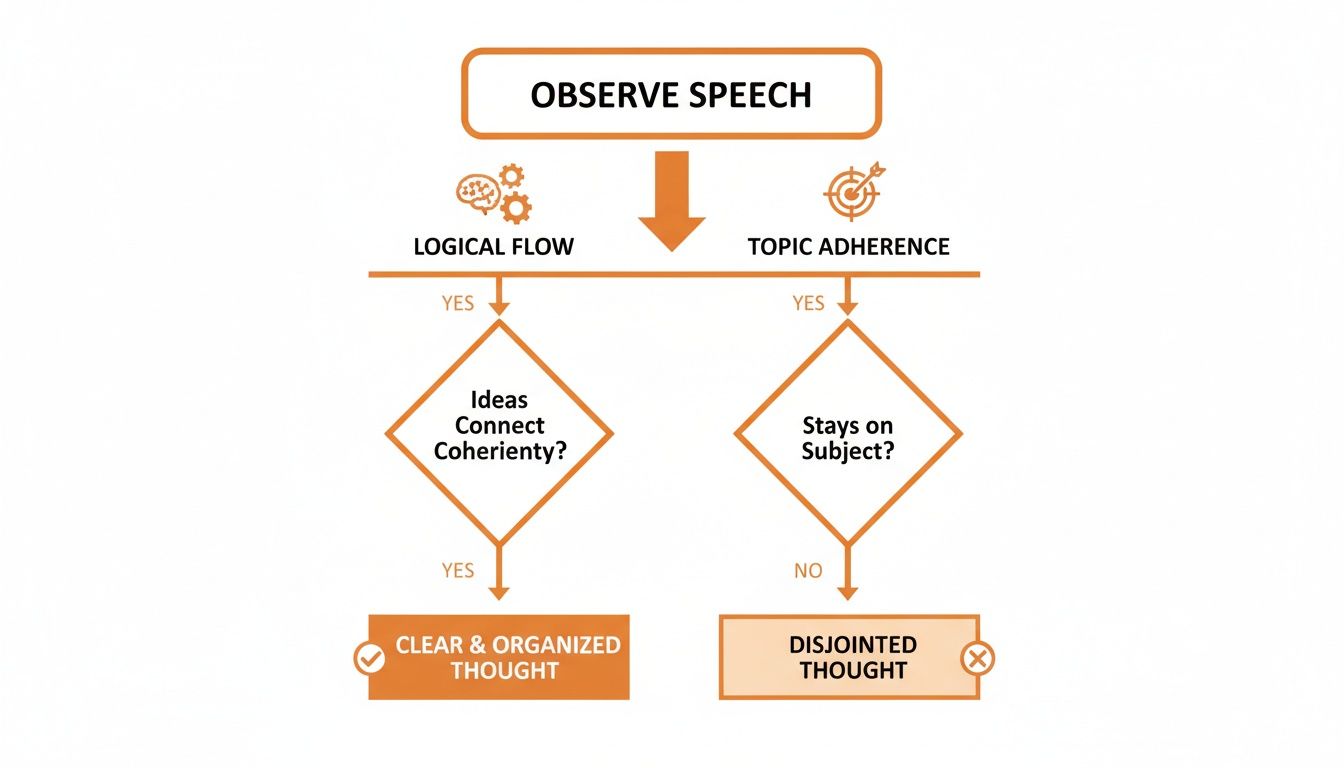
As you can see, simply listening allows a clinician to evaluate both the logical flow and topic adherence of a person's thoughts—key indicators of their thought process.
The goal is never to just administer a test for the sake of a score. The real value lies in selecting an instrument that directly addresses the clinical question at hand, whether it's screening for depression in a busy clinic or conducting a detailed cognitive workup for a complex case.
In the end, the choice of assessment tool shapes the entire clinical pathway. A PHQ-9 score might trigger a referral, while the results of a MoCA could lead to neuropsychological testing and a specific dementia care plan. This strategic selection turns the mental state assessment from a simple observation into a powerful engine for effective diagnosis and treatment planning.
Turning Assessment Results into Actionable Insights

The assessment is done, the tools have been put away, and the data is on the table. So, what’s next? A score on a form or a set of clinical observations is just raw information. The real clinical artistry begins when we turn those results into a meaningful story that guides effective, human-centred care.
A high score on the PHQ-9, for example, doesn't automatically equal a diagnosis of major depressive disorder. It's a single, important data point, but it only gains its true meaning when placed in a larger context. This is where clinicians move beyond a mechanical "test-and-score" approach.
The goal is to weave the findings into a complete picture that includes the individual’s personal history, their cultural background, and the specific reasons they sought help in the first place. This is how we transform abstract data into actionable insights for diagnosis and treatment planning.
Integrating Context for a Holistic View
To truly grasp what assessment results are telling us, we have to connect them with other sources of information. Think of it like assembling a puzzle—each piece gives you a small clue, but the full picture only emerges when you see how they all fit together.
For example, a clinician might note that a patient shows a "flat affect" (limited emotional expression) and speaks in a slow, quiet voice. On its own, this could point toward depression. But what if we learn that the patient comes from a cultural background where emotional restraint is a sign of respect and strength?
Suddenly, the interpretation shifts. The observation is still valid, but the meaning behind it is far more nuanced. The behaviour might not be a symptom of a disorder but a reflection of cultural norms. Overlooking this context could easily lead to a misdiagnosis. Actionable insight: Always ask questions like, "How are strong emotions typically expressed in your family or community?" to understand the cultural lens.
The Ethical Imperative of Cultural Humility
Avoiding cultural bias isn't just good practice; it's an ethical necessity in a mental state assessment. Many standardized tools were developed based on norms from specific populations, and they don't always apply universally. It's our responsibility as clinicians to approach every assessment with cultural humility.
This means actively thinking about how factors like language, religion, and social values might influence how a person presents themselves and responds during an assessment.
A truly effective assessment acknowledges its own limitations. No single test or observation can capture the full complexity of a human being. The clinician’s role is to use these tools as a starting point for a deeper, more collaborative understanding.
This collaborative approach is fundamental to building a strong therapeutic alliance. When patients feel their unique context is understood and respected, they're far more likely to engage with their treatment, which is essential for ensuring good continuity of care throughout their journey.
From Interpretation to Intervention
Once the results are properly contextualized, they become a powerful road map for treatment. A detailed assessment gives us the foundation for a nuanced diagnosis and, more importantly, a personalized care plan that addresses the individual’s specific needs.
Here’s how that translation works in practice:
Formulating a Diagnosis: The combined data helps us confirm or rule out specific conditions, moving from broad possibilities to a focused clinical diagnosis.
Guiding Treatment: If an assessment reveals significant cognitive struggles, the treatment plan might include cognitive remediation exercises. If it points to severe anxiety, the focus might shift to exposure therapy or relaxation techniques.
Building Alliance: Discussing the results with the patient demystifies the process and empowers them. It makes them an active partner in their own care.
To see how assessment results translate into practical, immediate interventions, it's helpful to explore resources that offer practical guidance for working with dementia patients and managing their behavior. This is a perfect example of how observational data directly informs on-the-ground care strategies.
Spotting the Red Flags: When to Refer for a Deeper Look
Knowing when a routine mental state assessment is hinting at something more serious is a core clinical skill. While many issues can be managed in primary care or general counselling, some signs should be an immediate trigger for a referral to a psychologist or neuropsychologist for a much deeper evaluation. These red flags tell us a more comprehensive look is needed to get the person the exact care they require.
Think of it like this: a family doctor can handle the common cold, but they send a patient with severe, ongoing chest pain straight to a cardiologist. The same logic applies here. Recognizing these warning signs isn't about jumping to a diagnosis; it's about seeing the need for a specialist who has the right tools to really dig in and figure out what’s going on.
When to Escalate Care
Certain signs and symptoms are clear signals that a standard mental state assessment is only the first step. Frontline professionals need to be on high alert for these indicators, as they often point to underlying conditions that demand specialized attention.
Here are some key red flags to watch for:
Sudden, Dramatic Personality Shifts: A person who was once outgoing and meticulous becomes withdrawn, suspicious, and disorganized without any obvious reason.
Significant Functional Decline: An individual can no longer manage day-to-day tasks like personal hygiene, paying bills, or holding down a job due to cognitive or emotional struggles.
Persistent Psychotic Symptoms: Experiencing hallucinations (seeing or hearing things that aren't there) or holding onto delusional beliefs that don't waver, even when presented with logical counter-arguments.
Severe Memory Loss: This is more than just misplacing keys. It’s about forgetting important recent events, getting lost in familiar places, or being unable to learn new information.
The challenge is often greater in communities where mental health care isn't well-integrated into general wellness. For instance, a 2025 study in the Caribbean by CARICOM and UNICEF found that a staggering 58% of young people reported a profound lack of hope for the future. Yet, mental health screenings are rarely part of routine check-ups, which leads to widespread underdiagnosis. You can discover more about these concerning regional trends in youth mental health, which really highlights why we need to get better at spotting these red flags early.
A referral isn't a failure of the initial assessment. It’s actually a success—it's the critical step that connects someone with the specialized expertise they need for a precise diagnosis and an effective treatment plan.
Making the Referral Process Smooth
Once you’ve spotted a red flag, the next move is to ensure a smooth transition to a specialist. The goal is to make this process feel seamless and supportive, not like a bureaucratic hand-off. A clear, confident referral builds trust and helps the individual feel cared for, not just passed along.
Actionable Tip: A Practical Referral Scenario
Imagine a family doctor seeing a 68-year-old patient. He’s well-groomed and pleasant but can’t recall what he had for breakfast or even the current year. The doctor’s initial mental state assessment immediately flags a significant cognitive deficit.
Instead of just giving him a specialist's number, the doctor says: "Your memory concerns definitely warrant a closer look from an expert. I'm referring you to Dr. Smith, a neuropsychologist who can do more detailed testing to understand exactly what’s happening. My office will help you get that appointment scheduled."
This approach does a few things really well: it validates the patient’s concerns, clearly explains the next step, and offers direct support. It turns a simple mental state check-up into the first step on a clear, well-supported care pathway. To see how technology can make this process even stronger, our team at Orange Neurosciences can show you how to weave objective cognitive data right into your clinical workflow.
How Digital Platforms Are Reshaping Assessments

The future of mental state assessment is already unfolding, and it’s driven by objective data that makes the whole process more engaging. While traditional methods will always have their place, they often lean heavily on a clinician's observations and a patient's own description of their struggles. Digital platforms are taking us beyond those limitations, giving us precise, data-backed cognitive profiles that add a whole new layer of objectivity to our work.
These tools can translate complex cognitive functions—things like attention, memory, and processing speed—into hard data. This offers a level of precision that’s almost impossible to get from paper-and-pencil tests alone. For clinicians, it means having solid, standardized information that sharpens diagnostic accuracy and helps build more effective treatment plans from the ground up.
Making Assessments More Engaging and Accurate
One of the biggest wins with digital assessment tools is how they make the process less intimidating for the person being assessed. Many platforms use gamified, adaptive interfaces that feel more like a series of interactive challenges than a clinical test. This simple design shift can make a world of difference in reducing patient anxiety, which is often a major hurdle to getting an accurate picture.
When someone is less stressed and more engaged, their performance is a truer reflection of their actual cognitive abilities. That leads directly to more reliable and valid results.
Technology is not replacing clinical judgment; it's augmenting it. By providing objective data streams, digital platforms empower clinicians to see subtle cognitive patterns and make more informed decisions, ultimately elevating the standard of patient care.
These adaptive systems are also smart enough to adjust the difficulty of tasks in real-time based on how the user is doing. This keeps the assessment challenging enough to measure abilities accurately but not so tough that it becomes frustrating. The outcome is a much richer, more nuanced set of data for the clinician to work with.
Uncovering Deeper Insights with Objective Data
Where digital platforms really shine is in their ability to track cognitive changes over time with incredible precision. They can pick up on subtle shifts in processing speed, attention, or memory that might otherwise go unnoticed in a standard clinical interview. This ongoing data gives us a powerful way to monitor how well a treatment is working or to track the progression of a condition.
Let’s look at a practical example of how this plays out:
Traditional Method: A clinician might check in with a patient about their memory every few months. The patient’s answer is subjective—coloured by their mood that day or recent experiences.
Digital Platform Method: A tool like OrangeCheck can run a quick, standardized cognitive test at regular intervals. It can precisely measure reaction times down to the millisecond and track tiny improvements or declines in specific memory functions.
This kind of granular data is invaluable. It lets a clinician see that, for instance, while a patient feels like their memory is the same, their processing speed has actually improved by 12% since starting a new therapy. This objective proof can validate a treatment approach or signal that an adjustment is needed long before the changes become obvious through observation alone. Platforms like ours are designed to provide exactly this kind of clarity. To learn more, see how Orange Neurosciences supports neurodiverse learners with digital therapy platform technology.
Integrating Technology into the Clinical Workflow
The true power of these tools comes to life when they fit seamlessly into existing clinical workflows. Modern platforms are built to give clinicians clear, easy-to-read reports that boil down complex cognitive data into actionable insights. This not only saves valuable time but also supports better, more confident decision-making.
Actionable Insight: Imagine getting an objective cognitive profile that flags specific areas of weakness before you even meet a patient. You can then structure your session to explore those areas directly, asking targeted questions like, "The assessment noted some difficulty with attention. Can you tell me about a time this week when you struggled to focus?" This data provides a solid starting point for a more focused, personalized care plan.
By blending the irreplaceable value of clinical expertise with the precision of data-driven technology, we can paint a more complete and accurate picture of an individual's mental state. It's about working smarter, not harder, to elevate patient care.
Frequently Asked Questions
Stepping into the world of mental health care can feel overwhelming, and it's natural to have questions. We’ve put together answers to some of the most common ones we hear about the mental state assessment process, hoping to bring some clarity and confidence to your journey.
How Long Does a Mental State Assessment Take?
That’s a tricky one because there’s no single answer. The time it takes really depends on why the assessment is being done and where it's happening.
For example, a quick check-in at your family doctor's office using a screener like the PHQ-9 might only take 10-15 minutes. But if you're in a specialized psychiatric setting for a comprehensive evaluation, the process could easily stretch to an hour or more to make sure every detail is covered.
Is an Assessment the Same as a Diagnosis?
Not quite, though they are closely linked. Think of the mental state assessment as the fact-finding mission—it’s like a detective gathering clues at a scene.
The findings from the assessment are just one critical piece of a much larger clinical puzzle. A formal diagnosis only comes after a clinician pieces everything together: the assessment results, the patient’s personal history, insights from family, and their own professional judgment.
Who Can Perform a Mental State Assessment?
A wide range of trained healthcare professionals can conduct a mental state assessment, which helps make this kind of care accessible across the system.
You might see any of these professionals performing an evaluation:
Psychiatrists and psychologists
Clinical social workers
Psychiatric nurses
General physicians and other medical doctors
The level of detail and focus of their assessment will naturally vary based on their specific training, their role, and the reason you're being evaluated in the first place.
Ready to move beyond subjective notes and bring objective cognitive data into your practice? Orange Neurosciences offers advanced tools that translate observations into clear, actionable insights, helping you make faster, more confident decisions for the people you support. Visit our website at https://orangeneurosciences.ca or email us to discover how our platform can transform your workflow.

Orange Neurosciences' Cognitive Skills Assessments (CSA) are intended as an aid for assessing the cognitive well-being of an individual. In a clinical setting, the CSA results (when interpreted by a qualified healthcare provider) may be used as an aid in determining whether further cognitive evaluation is needed. Orange Neurosciences' brain training programs are designed to promote and encourage overall cognitive health. Orange Neurosciences does not offer any medical diagnosis or treatment of any medical disease or condition. Orange Neurosciences products may also be used for research purposes for any range of cognition-related assessments. If used for research purposes, all use of the product must comply with the appropriate human subjects' procedures as they exist within the researcher's institution and will be the researcher's responsibility. All such human subject protections shall be under the provisions of all applicable sections of the Code of Federal Regulations.
© 2025 by Orange Neurosciences Corporation



