A Guide to Continuity of Care for Better Patient Outcomes
Oct 10, 2025
Think of a patient's journey through the healthcare or education system. It's rarely a straight line. Instead, it's a series of handoffs between different professionals, appointments, and treatment phases. Continuity of care is the practical strategy that ensures nothing gets dropped during these handoffs.
It's about weaving these separate moments into a single, coherent story where vital information is never lost and care plans stay on track. This simple idea—keeping everyone on the same page—is the key to preventing the kinds of gaps that can lead to poor outcomes. Ready to see how you can apply it?
What Is Continuity of Care Really About?

Imagine your healthcare journey is a relay race. Each runner—your family doctor, a specialist, a physical therapist, and even a school counsellor—must flawlessly pass the baton to the next. Continuity of care is the actionable teamwork that ensures this baton, which represents your unique health story, is never dropped.
It’s about much more than just seeing the same doctor every time. It’s about creating an uninterrupted flow of information and maintaining a consistent, evolving treatment plan. This level of coordination is the bedrock for building trust, improving safety, and getting better long-term results.
When care is fragmented, patients get stuck in a frustrating loop of repeating their medical history, undergoing duplicate tests, and trying to make sense of conflicting advice. True continuity of care smooths out all that friction.
The Core of Coordinated Care
At its heart, this concept is about creating a shared understanding of a person's needs over time. It makes sure that every professional involved has the complete picture, not just a tiny snapshot from a single appointment. Here are the actionable benefits:
Improved Patient Safety: With everyone working from the same information, the risk of medical errors like incorrect prescriptions or missed diagnoses plummets. For example, a shared electronic health record prevents a specialist from prescribing a medication that conflicts with one given by the primary doctor.
Enhanced Health Outcomes: Consistent management of chronic conditions and dedicated follow-up care simply leads to better results and fewer complications down the road.
Greater Patient Trust: When patients feel seen and understood by a coordinated team, they're far more likely to stick with their treatment plans and become active partners in their own care.
A Practical Example
Let's look at a child with ADHD who works with a paediatrician, a school psychologist, and a cognitive therapist. Without continuity of care, these professionals are working in silos. They might even create separate plans that unknowingly contradict each other.
But with a coordinated approach, they share progress reports and critical insights. The therapist’s data on the child's improving attention span can inform the paediatrician’s medication adjustments. At the same time, the school psychologist can provide real-world feedback on how the child is doing in the classroom.
This creates a unified strategy that supports the child from every possible angle. Understanding how we work to integrate these insights shows how technology can powerfully bridge these gaps. This seamless integration turns separate efforts into a collective force for much better outcomes.
The Three Pillars of Effective Care Continuity
To get a real handle on what makes continuity of care work, we need to look at its core structure. Imagine a sturdy, three-legged stool. It’s designed to provide stable, consistent support. But if even one leg is shaky, the whole thing becomes wobbly and unreliable. The person sitting on it won't feel very secure.
It’s the same with care. The three legs are known as relational, informational, and management continuity. Each one supports a different, but equally vital, part of a patient's or student's journey. When they work together, they build a foundation for coordinated care that closes dangerous gaps and helps people move forward.
Relational Continuity: The Human Connection
This is all about the ongoing, trusting relationship built over time between a person and their care provider. It’s the human element—the familiar face you know and trust, whether it's your family doctor, a dedicated therapist, or a school counsellor.
This bond isn't just about comfort; it's a powerful clinical asset. When a professional truly knows your history, your personality, and what matters to you, they can make far more insightful decisions. They'll notice subtle changes others might miss and offer advice that actually fits your life.
Practical Example: A child with a learning disability feels much safer opening up about their struggles with a school psychologist they've seen for years. That trust allows the psychologist to gather better information, which in turn leads to more effective strategies. It's a perfect example of how relationships strengthen continuity of care.
A consistent relationship with a care provider isn't just a preference; it's a proven factor in better health management. Studies show that patients with strong relational continuity are more likely to adhere to treatment plans and experience fewer hospitalisations.
Informational Continuity: The Complete Story
Next up is informational continuity. This pillar is focused on one thing: ensuring a person's complete and accurate history is available to every professional involved in their care, at every single step. It’s about creating one coherent story, not a jumble of scattered chapters.
This means no more repeating your entire history at every new appointment. It relies on the seamless transfer of key data—from test results and diagnoses to treatment notes and medication lists. When a specialist can instantly see the notes from a primary care physician, or a therapist can review a student's educational assessment, decisions become safer and much more informed.
Practical Example: A senior moving from a hospital back to a long-term care home. With strong informational continuity, the care home team gets their full medical records before they even arrive. They already know about medication allergies, recent procedures, and cognitive status, letting them build a safe and effective plan from day one.
This visual really clarifies how each of the three pillars contributes to a single, unified experience.
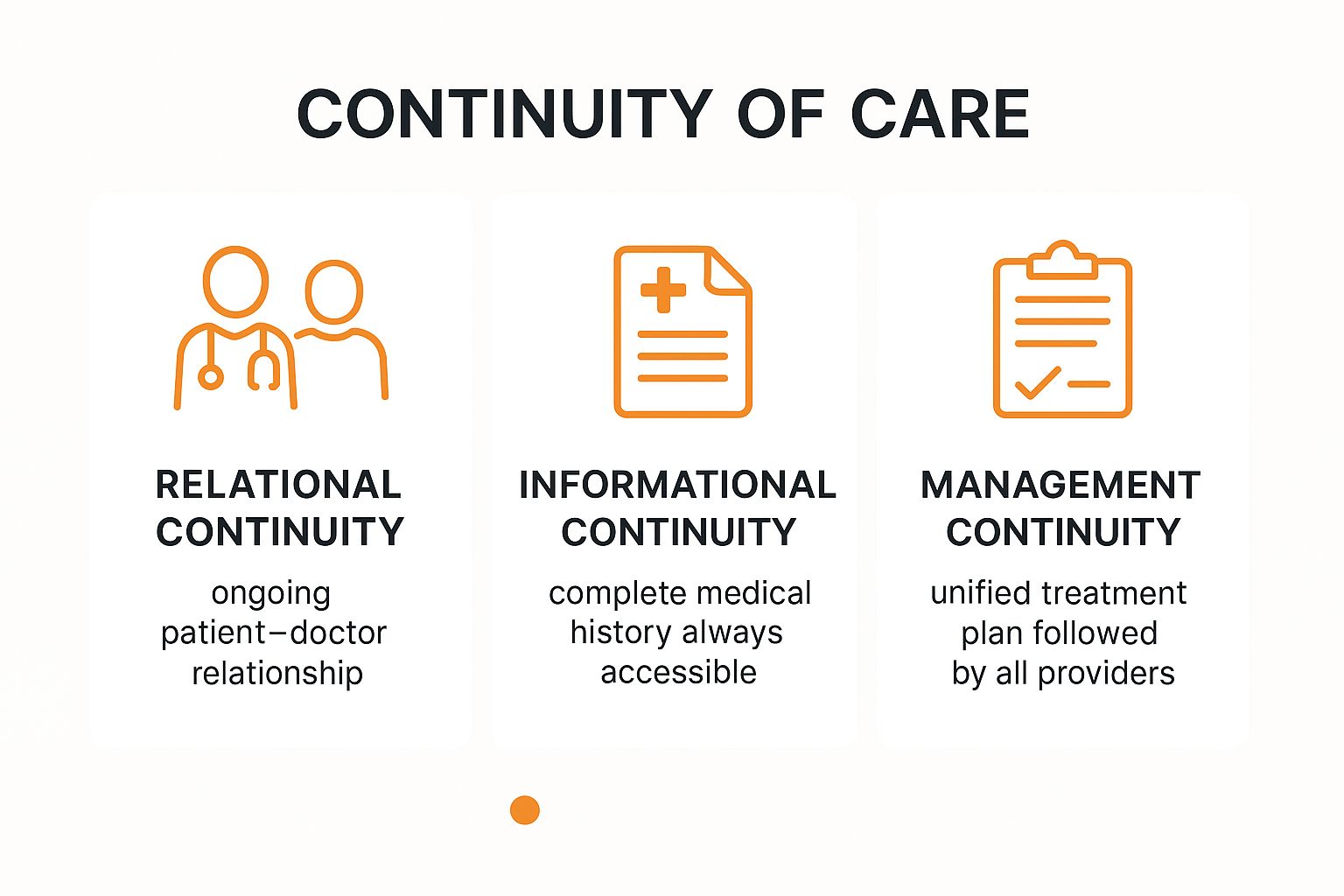
As the infographic shows, it’s the combination of focusing on relationships, data, and coordinated plans that creates a truly seamless journey for the patient or student.
Management Continuity: The Unified Plan
Finally, we have management continuity. This is where everything comes together to ensure all providers are following a single, coherent treatment plan. It’s absolutely critical for anyone with complex or chronic conditions who sees multiple specialists.
This pillar demands clear communication and solid agreement among all team members on the goals and methods of treatment. When management continuity is strong, a patient gets complementary advice, not conflicting instructions from their various providers. It’s about everyone rowing in the same direction.
To see how Orange Neurosciences provides the tools for this unified approach, visit our website or send us an email to learn more.
Comparing the Three Pillars of Continuity of Care
To make these concepts even clearer, let's break them down side-by-side. The table below outlines each pillar, its main goal, and how it looks in a real-world clinical or educational setting.
Pillar Type | Primary Focus | Practical Example |
|---|---|---|
Relational | Building a long-term, trusting relationship between an individual and their care team. | A student with ADHD consistently works with the same school counsellor over several years, building rapport that allows for open discussion of challenges. |
Informational | Ensuring all providers have access to a complete and up-to-date record of an individual’s history and care. | A patient's electronic health record, including notes from their GP, a psychiatrist, and a neurologist, is shared seamlessly among all three providers. |
Management | Coordinating care across different providers and settings to follow a single, consistent plan of action. | A care team for an elderly patient with dementia holds regular meetings to align on medication changes, therapy goals, and family support strategies. |
Ultimately, a patient's care is only as strong as the weakest of these three pillars. When all three are prioritized, the result is a system that feels supportive, intelligent, and truly centred on the individual.
How Coordinated Care Drives Better Results

When continuity of care is a priority, the impact goes way beyond theory and administrative checkboxes. The benefits are real, measurable, and deeply felt by patients, providers, and the healthcare system as a whole. It’s what turns the patient experience from a series of disconnected, often frustrating, appointments into a single, supportive journey toward better health.
This connected approach is a direct line to higher patient satisfaction. People feel heard and seen when they don’t have to recite their entire medical history at every single visit. A solid, ongoing relationship with a primary care provider builds trust, which in turn makes patients more likely to stick to treatment plans and take an active role in their own care.
That engagement leads to clearly better health outcomes, especially for anyone managing a chronic condition. For example, a patient with diabetes who sees the same doctor regularly is more likely to keep their blood sugar under control because their doctor can spot trends over time and adjust treatment proactively, preventing complications. The end result? Fewer complications and a much better quality of life.
The Financial and Clinical Impact
The ripple effects on the healthcare system are just as powerful, especially when it comes to the bottom line. Effective continuity of care is one of the best tools we have for preventing unnecessary medical treatments and boosting efficiency. When a care team is on the same page, the chances of redundant tests, conflicting prescriptions, and preventable hospital visits plummet.
For example, a strong relationship with a primary care doctor is directly linked to fewer emergency room trips and lower hospital readmission rates. Research out of California showed that patients who consistently saw the same primary care provider had a 2.1% higher chance of avoiding the emergency department and a 1.7% higher likelihood of having no hospitalizations at all. You can explore the full study on primary care adherence to dig into the data.
Continuity of care isn't a luxury; it's a critical investment in a more effective and sustainable healthcare system. By preventing costly complications and cutting down on redundant services, it delivers a powerful return in both financial savings and improved patient lives.
An Investment in Sustainable Healthcare
When you look at the evidence, it's clear. Prioritizing coordinated care creates a positive feedback loop with huge advantages. Here are actionable takeaways for your practice:
Better Chronic Disease Management: Consistent monitoring and adjustments lead to improved control over conditions like diabetes, hypertension, and asthma.
Reduced Medical Errors: A shared, deep understanding of a patient's history minimizes the risk of medication mix-ups and misdiagnoses.
Lower Healthcare Costs: Fewer emergency visits and hospital stays add up to significant savings across the entire system.
These benefits make continuity of care an essential strategy for any modern practice. For healthcare providers looking to put these ideas into practice, the next step is understanding how technology can support a unified care plan. By integrating objective cognitive data, for instance, clinicians can make sure every team member is working with the same insights, strengthening care management across the board. To see how this works, learn how Orange Neurosciences supports healthcare providers in building more connected and effective care pathways.
Overcoming Common Barriers to Seamless Care
While the goal of seamless care is a noble one, getting there is rarely a straight line. The reality is that many healthcare and educational systems are up against some serious roadblocks that break up the patient's journey, causing friction and frustration for everyone. The first step to building a better, more connected system is to call out these barriers for what they are.
One of the biggest culprits? Fragmented IT systems. Think about it: a family doctor’s electronic health record (EHR) can’t talk to a specialist’s system, which in turn can’t sync with a school's database. This traps critical information in digital silos. It turns patients into couriers, forcing them to repeat their stories and physically carry test results from one appointment to the next. Every time this happens, there's a risk that vital data gets lost in the shuffle.
This technological disconnect naturally leads to another major hurdle: poor communication. Without a standard way for providers to share updates, important insights fall through the cracks. The result is often an uncoordinated, and sometimes contradictory, care plan.
Navigating Systemic and Logistical Hurdles
Beyond the tech and communication gaps, patients themselves often run into a wall of logistical challenges. Trying to juggle appointments with multiple specialists, figuring out transportation, and managing complex medication schedules can be completely overwhelming. This is especially true for people dealing with chronic conditions or cognitive challenges. These aren't just minor inconveniences; they lead to missed appointments and patients not sticking to their treatment, which directly undermines continuity of care.
A practical example of a breakdown: An elderly patient is discharged from the hospital with a new heart medication, but the discharge summary isn't sent to their primary care doctor. Two weeks later, the doctor, unaware of the change, refills a previous prescription that interacts dangerously with the new one. This is where dedicated hospital discharge services can be invaluable, helping to prevent these disruptions by making sure there's a smooth and well-informed handover.
A patient's journey should feel like a well-coordinated relay, not a confusing maze. When systems fail to connect, the burden of navigating the maze falls on the patient, turning their path to recovery into an exhausting and often lonely effort.
Addressing Barriers on a Larger Scale
These challenges aren't just isolated incidents; they often point to much bigger systemic problems. Large-scale programs are working to close these gaps by creating more integrated delivery models. Take California's Medi-Cal managed care program, for instance. It’s the largest of its kind in the United States, and it's built around integrated service delivery for its over 10 million members. The whole point of programs like this is to improve continuity of care by coordinating different services under one unified plan, especially for those with the most complex needs. You can discover more about how Medi--Cal's structure supports integrated care and the difference it makes for patients.
Ultimately, breaking down these barriers comes down to a commitment to technology that can talk to each other, clear communication protocols, and logistics designed around the patient. To see how modern platforms can bridge these divides and support your practice, connect with the team at Orange Neurosciences. Our experts can show you how to build a truly seamless care journey for your patients.
How Technology Is Bridging Gaps in Patient Care

This screenshot isn't just a picture of a tablet—it’s a perfect example of modern technology turning complex cognitive data into something a care team can actually use. This is how we maintain strong continuity of care: by making information clear, shareable, and actionable.
Technology has become the essential connective tissue for a seamless patient journey. It's actively closing the communication and information gaps that have historically tripped up traditional healthcare, making sure everyone is working from the same playbook. These tools aren't just a nice-to-have anymore; they are fundamental to coordinated, effective care.
At the very centre of this shift are Electronic Health Records (EHRs). Think of an EHR as the single, authoritative source for a patient's entire health story, from lab results to a specialist's notes. When these systems can talk to each other, a patient's critical information travels with them, giving every provider the full picture. This is a game-changer for informational continuity and drastically cuts down the risk of errors.
Strengthening Connection and Management
Beyond just records, tools like patient portals and telehealth services have turned patients into active participants in their own care. Portals give people direct access to their own health info, test results, and schedules, which naturally gets them more engaged. Telehealth, on the other hand, knocks down geographical walls, making consistent follow-ups for chronic conditions not just possible, but practical.
This tech also makes a huge difference on the administrative side. Innovations in healthcare documentation automation, for example, can take a mountain of paperwork off a clinician's plate, ensuring vital patient information is recorded accurately and consistently across every setting.
Technology transforms continuity of care from a logistical headache into an achievable standard of practice. By creating a shared digital space, it ensures a patient's care plan stays consistent, coherent, and constantly up-to-date.
A Practical Example of Digital Therapeutics
Digital solutions are also making huge strides in management continuity, especially in cognitive health. This is exactly where platforms like Orange Neurosciences come in. Our digital therapeutic tools offer consistent, data-driven cognitive therapy that clinicians and educators can track from anywhere. This creates a cohesive care plan that doesn't stop, whether the patient is in a clinic, at school, or at home.
Here are the actionable benefits you can achieve:
Consistent Therapy Delivery: The platform serves up standardized, engaging cognitive exercises, which means no more guesswork or variation in treatment.
Real-Time Data Sharing: Clinicians and educators get objective progress reports as they happen, letting them make smart, timely adjustments to the care plan.
Remote Monitoring: This is absolutely crucial for keeping the momentum going between in-person appointments, closing those gaps where a patient's progress might otherwise stall.
With this approach, every member of the care team—from the clinician to the teacher to the parent—is working with the exact same objective data. To see what this looks like in the real world, you can explore our digital therapeutic solution and see for yourself how it builds a stronger foundation for continuity of care.
Frequently Asked Questions About Continuity of Care
To wrap things up, let's tackle some of the most common questions people have about achieving truly connected and effective care. This section is all about actionable insights to help you better understand and advocate for strong continuity of care.
How Can Patients Advocate for Better Continuity of Care?
As a patient or caregiver, you have a powerful voice. Here are three actionable steps you can take:
Be proactive. Ask your providers, "How do you communicate with the other specialists on my care team?" Don't hesitate to request copies of your own records and test results.
Designate a "quarterback". Choose a primary care provider to be the central point of contact for your health journey and ensure they are aware of all other specialists and treatments.
Prepare a summary. Keep a concise, one-page summary of your health history, current medications, and allergies. Bring it to every appointment to bridge information gaps, especially with new providers.
What Is the Difference Between Coordinated Care and Continuity of Care?
While they're closely related, these terms aren't interchangeable. Think of continuity of care as the seamless experience you have over time—often with the same trusted provider (that’s relational continuity) or through perfectly shared information (informational continuity). It's all about the consistency of your health journey.
Coordinated care, on the other hand, is the active process of organising all the different healthcare activities. It’s the behind-the-scenes teamwork that makes continuity possible, especially when multiple specialists and services are involved.
In short, coordination is the action of organising care, while continuity is the result—a smooth, connected patient experience without gaps or contradictions. You can't really have one without the other for high-quality outcomes.
How Does Continuity of Care Affect Vulnerable Populations?
For vulnerable populations—including seniors, children with special needs, and low-income families—continuity of care isn't just a "nice-to-have." It's absolutely critical. These groups often have to navigate incredibly complex systems with multiple providers, which makes them much more susceptible to falling through the cracks.
Events that strain public health systems really shine a light on these risks. For instance, during the COVID-19 pandemic, California's Medi-Cal program grew by 8%, adding over one million new enrollees in just nine months. This surge, impacting over 13 million Californians, underscored just how important robust continuity policies are for managing care when a vulnerable population grows so rapidly. You can learn more about Medi-Cal's enrollment trends and what they mean for public health.
What Role Does Technology Play in Rural Areas?
In rural or underserved communities, technology is an essential lifeline for maintaining continuity of care. Geographical distance often makes regular, in-person visits with specialists a huge challenge. This is where telehealth really steps in to fill the gap.
Here are practical ways technology helps:
Telehealth Consultations: These allow patients to have follow-up appointments and specialist consultations without having to travel long distances, ensuring they get consistent oversight.
Remote Monitoring Tools: These tools enable providers to track chronic conditions like diabetes or hypertension from afar, helping them catch potential issues before they become serious.
Shared Digital Records: This ensures that a local primary care provider and a specialist in a city hundreds of kilometres away are both working from the same up-to-date patient information.
These tools are crucial for bridging the distance, making high-quality, continuous care a reality no matter where a patient lives.
True continuity of care relies on consistent, objective data that every provider can access and understand. Orange Neurosciences provides the tools to build that foundation, turning fragmented assessments into a unified cognitive health journey.
Ready to close the gaps in your care workflow? Book a demo with Orange Neurosciences today.

Orange Neurosciences' Cognitive Skills Assessments (CSA) are intended as an aid for assessing the cognitive well-being of an individual. In a clinical setting, the CSA results (when interpreted by a qualified healthcare provider) may be used as an aid in determining whether further cognitive evaluation is needed. Orange Neurosciences' brain training programs are designed to promote and encourage overall cognitive health. Orange Neurosciences does not offer any medical diagnosis or treatment of any medical disease or condition. Orange Neurosciences products may also be used for research purposes for any range of cognition-related assessments. If used for research purposes, all use of the product must comply with the appropriate human subjects' procedures as they exist within the researcher's institution and will be the researcher's responsibility. All such human subject protections shall be under the provisions of all applicable sections of the Code of Federal Regulations.
© 2025 by Orange Neurosciences Corporation



