Concussion and Sleeping: Your Guide to Rest and Faster Recovery
Dec 26, 2025
That bone-deep exhaustion you feel after a concussion isn't just your body being tired. It’s a critical sign that your brain's number one recovery tool—sleep—has been disrupted.
The connection between a concussion and sleeping is incredibly tight; in fact, sleep problems are one of the most common and frustrating symptoms, hitting up to 90% of patients. Getting your sleep back on track isn't just a good idea; it's a non-negotiable part of any effective recovery plan.
The Unseen Struggle: Concussion And Your Sleep

Practical Example: Think about a student-athlete, weeks after a hard hit on the field, who can't seem to focus in class. They feel perpetually foggy and short-tempered, not because they aren't trying, but because they haven't had a single night of truly restorative sleep since the injury. Their grades slip, and they get benched, creating a cycle of stress that makes sleep even harder to find.
Or picture an office worker who, after a fender bender, now finds themselves fighting insomnia night after night. They stare at the ceiling for hours before finally drifting into a light, unsatisfying doze that leaves them feeling worse. The next day, they can't concentrate in meetings and make simple mistakes, putting their professional performance at risk.
These stories are all too common. A concussion sends the brain’s finely tuned systems into disarray, and the sleep-wake cycle is often one of the first and most significant casualties. This goes way beyond simply feeling tired. It's a fundamental roadblock to healing.
Why Sleep Is a Pillar of Concussion Recovery
When the brain gets injured, it kicks off a massive healing project that requires a tremendous amount of energy. Sleep is prime time for this critical repair work. During our deepest sleep cycles, the brain gets busy clearing out metabolic waste, cementing memories, and working to get back to business as usual.
But when a concussion throws a wrench in this process, recovery can grind to a halt. This creates a vicious cycle where poor sleep makes other concussion symptoms flare up, like:
Intensified Headaches: A lack of sleep is a major trigger for migraines and tension headaches.
Cognitive Fog: Without proper rest, that feeling of mental sludge—difficulty concentrating and remembering things—gets much worse.
Emotional Dysregulation: Irritability, anxiety, and wild mood swings are almost always amplified by sleep deprivation.
Actionable Insight: Actively managing sleep is not just a helpful tip—it's a core component of effective treatment. Start tonight by creating a simple "wind-down" routine an hour before bed: dim the lights and put away all screens.
Moving Beyond Guesswork in Healing
For clinicians, parents, and patients, recognizing this link is the crucial first step. The next is figuring out how to navigate the road to recovery with real clarity. How can you be sure that sleep interventions are actually working? How do you know if cognitive function is truly getting better?
The tricky part about concussions is that so many symptoms, like fatigue or brain fog, are subjective. This is where modern tools are changing the game. By learning about the long-term effects of a concussion, you can better appreciate why objective monitoring is so important.
Objective cognitive monitoring gives us a data-driven way to watch the brain's healing journey unfold. Instead of just relying on how someone feels, these assessments provide concrete measurements of attention, processing speed, and other key brain functions. This data offers clinicians and families a clear, unbiased picture of recovery, helping to fine-tune treatment decisions and pave a safer path back to school, work, and life.
Why a Concussion Rewires Your Brain's Sleep Controls
Imagine your brain's sleep-wake system is like a finely tuned orchestra. Every part works in perfect harmony, creating restful nights and energetic days. A concussion is the equivalent of a sudden, deafening crash, throwing the entire orchestra into disarray. This is the neurobiological reality of why getting a good night's sleep after a concussion can feel next to impossible.
This isn't just about feeling a bit groggy; it's a fundamental rewiring of your brain's most basic controls. The injury directly impacts the complex systems that tell you when to feel sleepy and when to feel awake. All of a sudden, the conductor of your internal orchestra has lost the sheet music, and every instrument is playing out of sync.
The Melatonin Misfire
One of the first casualties in this neurological chaos is melatonin, often called the "sleep hormone." Your brain’s pineal gland is meant to produce melatonin when it gets dark, sending a clear signal that it's time to wind down. But a concussion throws a wrench in this delicate process, causing the brain to produce too little melatonin or release it at completely the wrong times.
Practical Example: A teenager recovering from a sports injury lies wide awake at 2 a.m., staring at the ceiling. Their brain simply isn't getting the "time for sleep" signal it needs, leaving their sleep cycle adrift. This isn't a behavioural issue; it's a direct consequence of the injury messing with the natural rhythm of their hormones.
The struggle with sleep post-concussion is a huge problem, especially for young athletes. Data from California reveals a sharp increase in sports-related brain injuries, with countless young people reporting severe sleep problems during recovery. In Riverside County, for example, sports-related TBI hospitalizations hit a high in 2021, and football was responsible for the highest rate of emergency department visits. These injuries frequently lead to wrecked sleep architecture—like reduced REM sleep, which is critical for brain healing and cognitive recovery. You can dig into the detailed findings in the full Riverside County report on sports-related TBIs.
Damage to the Brain's Control Tower
Your brainstem and hypothalamus are the central command centre for all things sleep. Unfortunately, these structures are incredibly vulnerable during a concussion, as the rotational forces of the impact can stretch and damage their delicate neural connections. When this "control tower" is damaged, its ability to manage your sleep-wake cycle is seriously undermined.
This damage often shows up in a few key ways:
Insomnia: You can't fall asleep or stay asleep because the "off" switch for being awake is broken.
Hypersomnia: You feel an overwhelming need to sleep all the time because the "on" switch for alertness isn't working right.
Fragmented Sleep: You wake up constantly throughout the night, never getting into the deep, restorative stages of sleep your brain needs to heal.
Actionable Insight: A concussion doesn't just make you feel tired; it physically damages the parts of the brain that orchestrate the entire process of falling asleep, staying asleep, and waking up refreshed. Understanding this can help you be more patient with your body's recovery process.
Inflammation and Neurotransmitter Interference
After a concussion, the brain kicks off an inflammatory response to start healing. While this is a good and necessary part of recovery, the inflammation can also interfere with neurotransmitters—the chemical messengers that let brain cells talk to each other.
Key neurotransmitters for sleep, like serotonin and GABA (gamma-aminobutyric acid), get thrown completely out of balance. Serotonin helps regulate sleep cycles, and GABA has a calming effect that helps you drift off. When inflammation disrupts their normal flow, you're left with a brain that is chemically wired for wakefulness and anxiety, even when your body is desperate for rest.
This complicated mix of hormonal disruption, structural damage, and chemical imbalances is precisely why concussion and sleeping problems are so deeply connected. Understanding these root causes is the first real step toward finding effective ways to get your brain's natural rhythm back on track. For a deeper understanding of how we can help you navigate this journey, connect with us at Orange Neurosciences.
Recognizing The Common Post-Concussion Sleep Disorders
When someone has a concussion, just saying "I'm having trouble sleeping" is a huge understatement. The reality is often much more specific than general fatigue, and figuring out the exact nature of the problem is the first real step toward finding a solution.
The neurological ripple effect from a concussion can trigger very distinct sleep disorders, each with its own signature. Naming these patterns helps everyone—patients, parents, and therapists—move beyond vague complaints and toward an actionable plan for recovery.
This infographic gives a clear picture of how a concussion throws a wrench into the core systems that regulate our sleep.
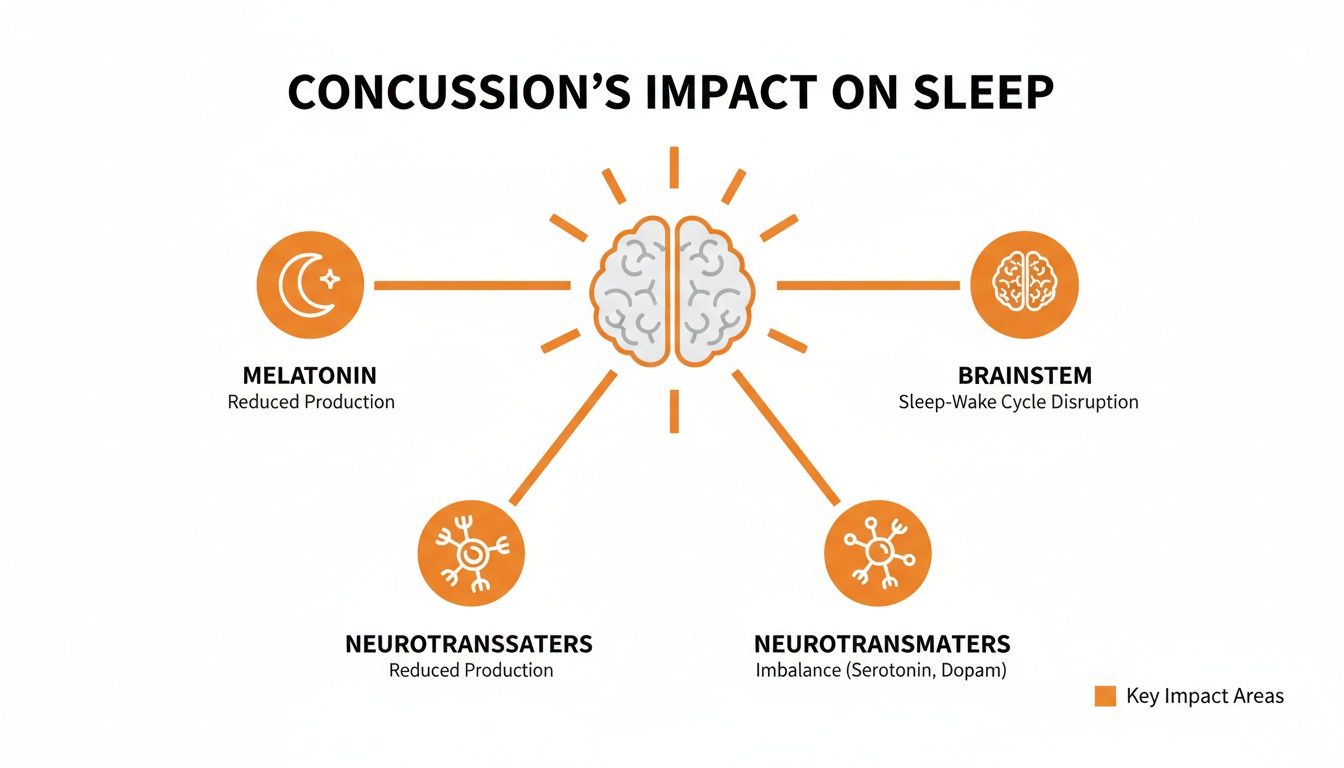
As you can see, the injury creates a domino effect. It messes with chemical messengers like melatonin and disrupts the brain's fundamental sleep control centres.
To help you identify what might be going on, here’s a breakdown of the most common sleep disturbances we see after a concussion.
Recognizing Post-Concussion Sleep Disturbances | ||
|---|---|---|
Sleep Problem | Common Symptoms | Potential Underlying Cause |
Post-Traumatic Insomnia | Difficulty falling asleep, waking up frequently, or waking up too early and being unable to fall back asleep. | Brain inflammation, neurotransmitter imbalance (GABA, glutamate), pain, or anxiety. |
Circadian Rhythm Disorders | Feeling wide awake late at night and struggling to wake up in the morning (Delayed Sleep Phase); feeling sleepy in the evening and waking too early. | Disruption to the suprachiasmatic nucleus (the brain's master clock) and melatonin production. |
Hypersomnia | Excessive daytime sleepiness, sleeping much longer than usual (e.g., 10+ hours) but still feeling unrefreshed. | Damage to brainstem areas that regulate wakefulness (e.g., the reticular activating system). |
These aren't just labels; they represent real, disruptive experiences that significantly impact a person's ability to heal. Let's look a little closer.
Post-Traumatic Insomnia
This is, by far, the most common sleep complaint after a head injury. But insomnia isn't a one-size-fits-all problem; it can show up in a few different ways, and it's important to spot the differences.
Some classic signs include:
Sleep-onset insomnia: Lying in bed for what feels like hours, mind racing, completely unable to drift off.
Sleep-maintenance insomnia: Waking up over and over again during the night and finding it tough to get back to sleep.
Early-morning awakening: Waking up way too early—say, at 4 a.m.—and that’s it, you're up for the day.
Practical Example: Someone recovering from a fall might pass out from exhaustion but then wake up every two hours, feeling alert. Their total sleep time might look okay on paper, but the quality is so fragmented that they never reach the deep, restorative stages needed for brain repair. They wake up feeling completely drained.
Actionable Insight: It's not just about the quantity of sleep; it's about the quality. A concussion can fracture your sleep architecture. To track this, keep a simple sleep diary for a week: note when you go to bed, when you wake up, how many times you wake up during the night, and how you feel in the morning.
Circadian Rhythm Disorders
A concussion can send your internal body clock, or circadian rhythm, into total chaos. Your brain stops getting the right signals for when to be awake and when to sleep, creating a huge mismatch between your internal schedule and the 24-hour day.
A textbook example, especially in adolescents, is Delayed Sleep Phase Syndrome (DSPS).
Practical Example: A teenager who always went to bed around 10 p.m. now finds it impossible to fall asleep before 3 a.m. after a soccer concussion, no matter how tired they are. Getting up for school becomes a daily battle, leading to missed classes and a thick brain fog that won't lift. This isn't laziness or bad habits—their internal clock has been physically shifted hours later.
Hypersomnia: Overwhelming Daytime Sleepiness
While insomnia is about a lack of sleep, hypersomnia is the exact opposite: an excessive, overwhelming need for it. This isn't just feeling tired after an injury; it's a persistent, intrusive sleepiness that gets in the way of everything.
Practical Example: An adult might find themselves needing 12 hours of sleep a night but still feel an irresistible urge to nap all day at work. They might doze off in meetings or at their desk, not out of boredom, but because their brain's alertness signals are simply not working right.
Keeping a careful record of these symptoms is crucial. For anyone looking to systematically track their progress, using a structured tool like a post-concussion symptom questionnaire can provide clear, invaluable data to share with your healthcare provider.
Practical Strategies To Reclaim Your Sleep
Knowing why your sleep is a mess after a concussion is one thing, but knowing how to fix it is where the real power lies. Think of this as your playbook for getting better sleep, filled with proven strategies designed for a brain that’s actively healing. This isn't about generic sleep tips; it's about targeted, non-pharmacological approaches that genuinely support your recovery.
First things first, reframe how you think about bedtime. Forget an abrupt "lights out." Instead, treat the last hour before bed as a dedicated "wind-down" period. This slow, gentle transition is crucial for an extra sensitive brain.
Building Your Concussion-Friendly Sleep Routine
A solid, structured routine signals to your brain that it’s time to shut down. The key here is consistency—even on weekends. This helps reset your internal body clock.
Here’s a practical, step-by-step wind-down hour you can start tonight:
60 Minutes Before Bed: Dim the lights. Switch off bright overheads and use warm lamps instead. This is your cue to turn off all screens—phones, tablets, and TVs. The blue light they emit actively suppresses your body's melatonin production.
45 Minutes Before Bed: Choose a calming, screen-free activity. Listen to gentle music, a podcast, or an audiobook. Reading a physical book is another great option.
30 Minutes Before Bed: Try some gentle stretching or mindfulness exercises. Focus on releasing tension in your neck and shoulders. A warm (not hot) bath can also be fantastic, as the drop in body temperature afterwards helps trigger sleepiness.
15 Minutes Before Bed: Make your bedroom a sleep sanctuary. It must be cool, dark, and quiet. Use blackout curtains, an eye mask, or a white noise machine if needed.
This deliberate process helps ease your brain out of its daytime "go-go-go" mode and into a state that’s ready for sleep.
Actionable Insight: The goal of a wind-down routine is not to force sleep, but to create the ideal conditions for sleep to happen naturally. It’s about gently guiding your brain toward rest, not demanding it.
Introducing Cognitive Behavioural Therapy for Insomnia (CBT-I)
For many people, good sleep hygiene isn't enough. When insomnia becomes a persistent problem, Cognitive Behavioural Therapy for Insomnia (CBT-I) is the gold-standard treatment. It's a structured program that helps you identify and change the thoughts and behaviours that are wrecking your sleep.
While you'll get the best results working with a therapist, you can start applying its core principles tonight. Two of the most powerful techniques are stimulus control and sleep restriction.
1. Actionable Tactic: Stimulus Control Therapy The goal is to rebuild the connection between your bed and sleep—and only sleep.
Rule 1: Only get into bed when you are actually sleepy. Tossing and turning teaches your brain that bed is a place for frustration.
Rule 2: If you're still awake after 20-30 minutes, get out of bed. Go to another dimly lit room and do something quiet and relaxing (like reading) until you feel sleepy again, then return to bed.
Rule 3: The bed is for sleep and intimacy only. No working, eating, or scrolling on your phone in bed.
2. Actionable Tactic: Sleep Restriction Therapy This sounds counterintuitive but is incredibly effective. It involves limiting your time in bed to roughly the number of hours you're actually sleeping. This builds up a powerful "sleep drive" and reduces time spent lying awake. For instance, if you're in bed for eight hours but only sleeping for five, a therapist might have you start by restricting your time in bed to just five or five-and-a-half hours to help consolidate that sleep.
These strategies take patience but are highly effective at breaking the vicious cycle of insomnia. To help your recovery even more, it's a great idea to explore a range of established methods for better sleep. You can find many proven techniques for natural and restful sleep that work well alongside these concussion-specific strategies.
Putting these methods into practice can make a huge difference in your sleep quality, which is absolutely fundamental to a faster, fuller recovery. If you're looking for a more comprehensive approach to your healing, learn about our integrated neurorehabilitation programs that tackle every aspect of concussion recovery.
Using Objective Data To Guide Your Recovery Journey

How do you really know if a concussion is healing properly? Simply asking someone how they feel can be a shot in the dark. Statements like "I feel a bit better today" are useful, but fatigue and brain fog are notoriously unreliable narrators, especially when poor sleep is muddying the waters.
This is where objective data changes everything. It cuts through the guesswork, offering a clear, unbiased look at how the brain is actually performing.
Moving Beyond "How You Feel"
Practical Example: A student-athlete insists they feel "fine" and is itching to get back on the field. On the surface, they seem ready. But what if an objective cognitive test shows a major lag in their processing speed and attention? These are classic signs that poor sleep is still holding their brain's recovery hostage.
This happens all the time, and it’s one of the biggest risks in concussion management. Making crucial decisions about returning to play, work, or school based on feelings alone can send someone back too soon. This not only risks re-injury but can drag out the entire recovery timeline.
Actionable Insight: Relying solely on how you feel is like navigating without a map. Objective data provides the precise coordinates needed to guide a safe and effective recovery, ensuring that progress is real and measurable.
The Power of AI-Powered Cognitive Assessments
This is where modern tools come in. AI-powered cognitive assessments give us the precision needed to track recovery with real numbers, not just feelings. These platforms zero in on the key cognitive functions that take a direct hit from poor sleep after a concussion.
They can precisely measure functions like:
Attention and Concentration: How well can you actually focus on a task without your mind wandering? A sleep-deprived brain struggles immensely with this.
Processing Speed: This is how quickly you can take in information, make sense of it, and react. It's often one of the first things to slow down when sleep is disrupted.
Executive Function: This covers higher-level skills like problem-solving, planning, and decision-making—all of which need a well-rested brain to function properly.
Making Smarter Decisions with Data
With this clear, actionable data, clinicians, therapists, and families can build a much more personalized and effective care plan. You can see, in black and white, whether sleep interventions are actually working by watching cognitive scores improve over time.
This data-driven approach leads to smarter, safer decisions. It provides the concrete evidence needed to guide return-to-play protocols and back-to-work timelines, making sure the brain has truly regained its functional capacity.
Of course, beyond specific concussion-related strategies, good sleep hygiene is fundamental. For a deeper dive into the role of sleep in faster recovery, exploring broader tactics can be incredibly helpful. When you combine objective data with proven sleep strategies, you create a powerful formula for a much smoother and more successful recovery.
Your Roadmap To Better Sleep And A Faster Recovery
Recovering from a concussion often feels like running a marathon. Quality sleep is your strongest ally in getting back on your feet—and sooner than you might think.
In this guide, we’ve unpacked how concussions can throw your sleep off balance, shown you how to identify specific problems, and offered practical tactics to tackle them head-on.
Most importantly, we’ve highlighted the power of objective data to guide each step of your healing. Leaving recovery to guesswork can prolong symptoms and raise the risk of setbacks.
Take The Next Step In Your Recovery
Sleep disruptions don’t have to be permanent. The strategies we’ve covered set a clear path forward, but real progress comes from applying them with precision.
Whether you’re a clinician, therapist or family member supporting someone’s recovery, vague feelings of fatigue won’t answer critical questions about returning to school, sports or work. For a structured approach that brings clarity and confidence, explore our complete concussion management guide.
Objective cognitive data removes the ambiguity from concussion recovery.
It offers clear, unbiased evidence to track healing, assess sleep interventions and make safer, more informed decisions.
We encourage healthcare professionals and families to experience how the Orange Neurosciences platform delivers:
Precise cognitive profiles for each patient
Data-driven insights to tailor sleep and activity plans
Real-time tracking to verify progress
Stop guessing and start measuring. Visit our website or email us to discover how our neurocognitive assessments can transform your concussion care and build a truly effective roadmap to recovery.
Your Questions Answered
Trying to navigate the aftermath of a concussion is confusing enough without adding sleep problems to the mix. Let's clear up some of the most common questions we hear, giving you practical answers to guide your recovery.
How Long Will My Sleep Be Messed Up After a Concussion?
This is the million-dollar question, and the honest answer is: it varies. For some people, sleep patterns snap back to normal within a few days or weeks. But for others, especially if post-concussion syndrome sets in, these issues can drag on for months.
Actionable Insight: You can shorten that recovery window by being proactive. Start implementing a rock-solid sleep hygiene routine and ditching screens before bed tonight. If your sleep is still a mess after a few weeks, or it’s actually getting worse, that's your cue to get professional help. For instance, if a month has passed and you're still waking up multiple times a night, it's time to call the doctor.
Key Takeaway: A few weeks of choppy sleep is one thing, but problems that stick around or intensify are not. Don't just try to "wait it out." Your brain needs restorative sleep to heal, and it’s okay to ask for help to get there.
Is It Okay to Use Sleeping Pills After a Concussion?
Tread very, very carefully here. It’s tempting to reach for a quick fix when you're staring at the ceiling at 3 a.m., but many over-the-counter and prescription sleep aids can actually get in the way of your brain's healing. Some medications can suppress the deep, restorative stages of sleep—the very stages your brain needs most for repair. Others just mask the underlying problem that really needs to be addressed.
Actionable Insight: You must consult a physician who understands brain injury before taking any new sleep medication. Your first line of attack should always be non-medication strategies. Instead of reaching for a pill, try building a "wind-down" hour into your evening. Put on some calm music or a podcast, dim the lights, and just let your brain gently transition toward rest. It’s a simple change that lets you avoid the potential downsides of medication.
When Should I See a Doctor About My Sleep Issues?
It's vital to know when to raise the red flag. A little bit of sleep disruption right after the injury is expected, but certain signs mean it's time for a professional to step in.
Book an appointment with your doctor if you're experiencing any of these:
You've tried, but nothing's changing: You've been diligent with sleep hygiene for two weeks and see zero improvement.
The disruption is severe: We're talking about being completely unable to fall asleep for nights on end.
Other symptoms are getting worse: Your sleep problems are happening alongside escalating headaches, major mood swings, or worsening confusion and brain fog.
Actionable Insight: Be your own best advocate. A great practical step is to keep a simple sleep diary for a week before your appointment. Jot down when you go to bed, how many times you wake up, and how you feel the next morning. This gives your doctor real data to work with and helps them create a better plan for you. Getting the right support early on can make all the difference.
Navigating the complexities of concussion recovery requires more than just guesswork. Orange Neurosciences provides the objective data needed to create a clear, effective, and data-driven path to healing.
Discover how our AI-powered cognitive assessments can transform your approach to concussion care. Visit https://orangeneurosciences.ca to learn more and request a demo today.

Orange Neurosciences' Cognitive Skills Assessments (CSA) are intended as an aid for assessing the cognitive well-being of an individual. In a clinical setting, the CSA results (when interpreted by a qualified healthcare provider) may be used as an aid in determining whether further cognitive evaluation is needed. Orange Neurosciences' brain training programs are designed to promote and encourage overall cognitive health. Orange Neurosciences does not offer any medical diagnosis or treatment of any medical disease or condition. Orange Neurosciences products may also be used for research purposes for any range of cognition-related assessments. If used for research purposes, all use of the product must comply with the appropriate human subjects' procedures as they exist within the researcher's institution and will be the researcher's responsibility. All such human subject protections shall be under the provisions of all applicable sections of the Code of Federal Regulations.
© 2025 by Orange Neurosciences Corporation



