Your Guide to the Post Concussion Symptom Questionnaire
Oct 19, 2025
A post-concussion symptom questionnaire is a standardized checklist that helps you and your doctor keep a close eye on your symptoms after a head injury. Think of it less like a test you can pass or fail and more like a detailed weather report for your brain's recovery. It gives you a structured way to communicate precisely how you're feeling, capturing everything from headaches to that frustrating mental fog. For you, it's an actionable tool to track progress and identify triggers. For your doctor, it's the data needed to create a recovery plan that's truly tailored to you.
Understanding the Post Concussion Symptom Questionnaire
After a head injury, just trying to describe your symptoms can feel completely overwhelming. Words like "dizzy," "foggy," or "irritable" are subjective and can mean different things to different people. A post-concussion symptom questionnaire takes these feelings and translates them into objective, measurable data. It's a surprisingly simple yet incredibly powerful tool for both patients and healthcare providers.
To get a clear picture of what it is, it helps to understand the difference between a survey and a questionnaire, since people often use the terms interchangeably. At its heart, a questionnaire is a set of specific questions used to gather data from one person—which is exactly how this tool works in a clinical setting.
Key Symptom Categories
This tool brings order to what can feel like a chaotic mix of symptoms by sorting them into clear, manageable categories. This structure is key to making sure nothing gets overlooked during an assessment.
The symptoms are typically organized into clusters to provide a comprehensive view of a patient's experience.
| Common Symptom Clusters Assessed in a PCSQ |
| :--- | :--- |
| Symptom Cluster | Examples of Symptoms |
| Physical | Headaches, nausea, dizziness, sensitivity to light/noise, balance issues |
| Cognitive | Difficulty concentrating, memory problems, feeling slowed down, mental fog |
| Emotional | Irritability, sadness, anxiety, feeling more emotional than usual |
| Sleep-Related | Drowsiness, trouble falling asleep, sleeping more or less than usual |
By breaking symptoms down this way, clinicians can pinpoint which areas are most affected by the concussion.
By rating the severity of each symptom—for example, on a scale from 0 for none to 6 for severe—you create a detailed snapshot of your condition at a specific moment. This is especially helpful for tracking your recovery over time. For example, if your "sensitivity to light" score drops from a 5 to a 2 after a week of limiting screen time, that’s actionable proof that your strategy is working. Seeing that progress gives your care team clear, undeniable evidence of improvement.
This structured approach takes the guesswork out of recovery. It turns subjective feelings into concrete data, empowering your care team to see patterns, measure progress, and adjust your treatment plan effectively.
The widespread use of these questionnaires in Canadian clinics really highlights their importance. For instance, a Quebec-based study used symptom scales to identify patients struggling with persistent issues like dizziness, neck pain, and cognitive difficulties. The regular use of these tools in both research and daily clinical care across Canada shows just how vital they are for managing concussions.
To see how this kind of data feeds into a deeper analysis of brain function, check out our guide on what is a cognitive assessment.
Common Types of Questionnaires Your Doctor Might Use
When a doctor hands you a post-concussion symptom questionnaire, it might just look like another form to fill out. But these aren't generic checklists. Think of them like specialized tools in a carpenter's toolkit—each one is designed for a specific job. Knowing which tool your clinician is using, and why, helps you become a more active partner in your own recovery.
Two of the most common questionnaires you'll likely encounter are the Post-Concussion Symptom Scale (PCSS) and the Rivermead Post-Concussion Symptoms Questionnaire (RPQ). Both track your symptoms, but they come at it from slightly different angles.
The Post-Concussion Symptom Scale (PCSS)
The PCSS is a real workhorse in sports medicine, and for good reason. It’s direct, clear, and gets right to the point. The form lists 22 common concussion symptoms and simply asks you to rate the severity of each one on a scale from 0 (none) to 6 (severe).
This sharp focus on severity makes it perfect for tracking symptoms right after an injury and for making those crucial return-to-play decisions for athletes. It’s like taking a high-resolution snapshot of your symptoms at a specific moment in time.
What the PCSS is for: To quickly and effectively measure the severity of a wide range of concussion symptoms. It's ideal for acute injury assessment and monitoring progress, especially in a sports medicine setting.
The Rivermead Post-Concussion Symptoms Questionnaire (RPQ)
The RPQ, on the other hand, steps back to look at the bigger picture. It asks about 16 common symptoms, but the question is framed very differently. Instead of just rating severity, it asks you to compare how you feel now to how you felt before your injury. The rating scale, from 0 (not experienced at all) to 4 (a severe problem), is all about the impact on your life.
This approach gives a much richer, more personal picture of your recovery. It’s less about the raw intensity of a headache and more about how that headache is getting in the way of your work, your family time, and your ability to live your life normally. A practical example: a headache might score a "3" on the PCSS for severity, but on the RPQ, it could score a "4" because it's so disruptive it prevents you from reading your emails or joining a family dinner.
The infographic below gives a quick visual on how a clinician might decide between these two primary tools.
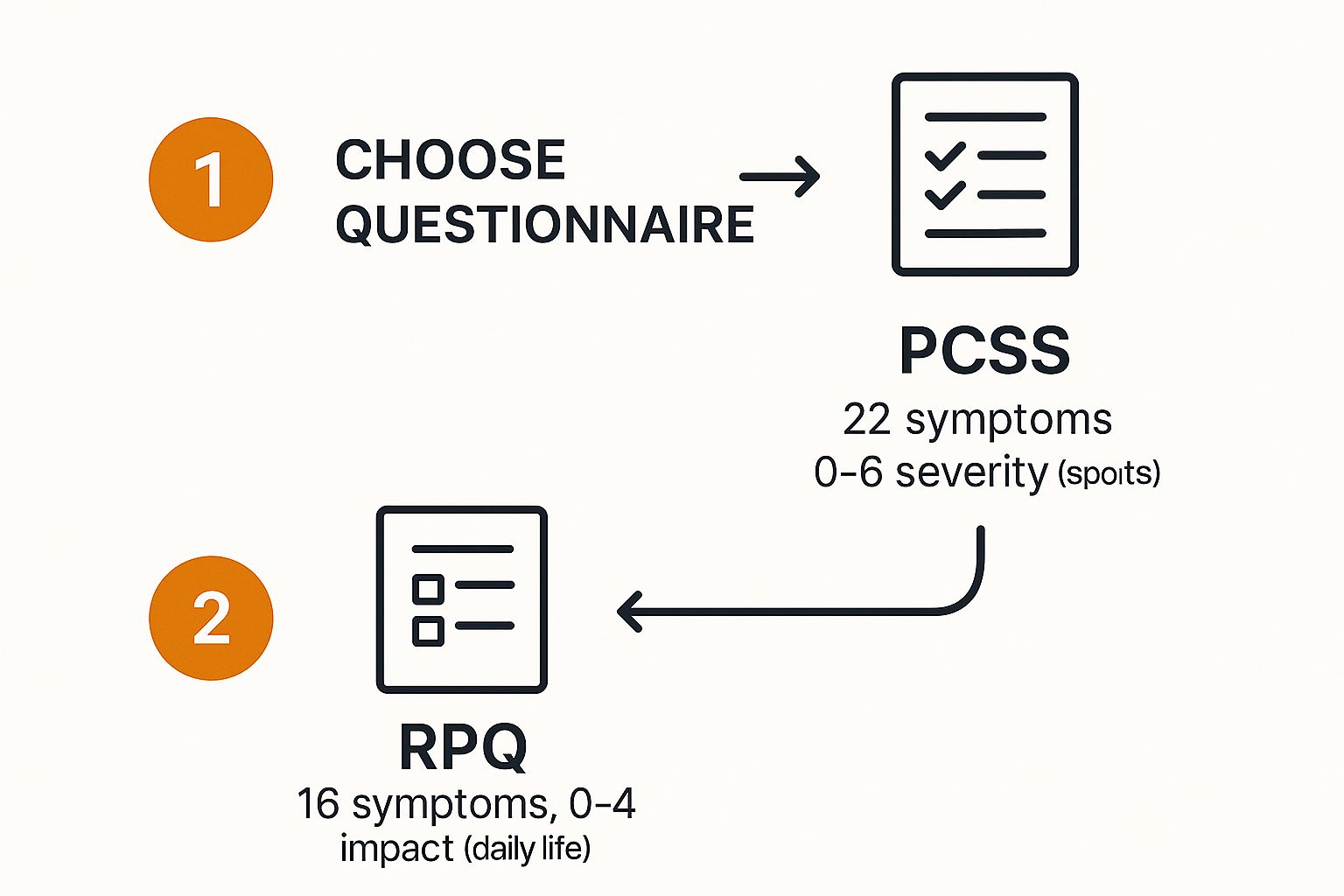
As you can see, the choice often boils down to the clinical setting and goals—PCSS for tracking symptom severity in sports, and RPQ for understanding the real-world impact in broader clinical care.
In Canadian clinical and research settings, the RPQ is a highly respected tool. It even breaks down the symptoms into strategic clusters. The first three items—headaches, dizziness, and nausea—form what's called the RPQ-3. The remaining 13 items make up the RPQ-13. A high score on that initial RPQ-3 can be an early flag for clinicians that a patient needs closer monitoring.
Of course, understanding your symptoms is just one piece of the puzzle. To see how this subjective feedback fits into a complete picture of brain health, take a look at our overview of cognitive assessments. You'll learn how we combine what you tell us with objective measurements to guide recovery.
How to Fill Out and Score the Questionnaire
At first glance, a post-concussion symptom questionnaire might seem a bit clinical, maybe even intimidating. But it's really just a structured way for you to communicate exactly how you're feeling. Think of it less like a test and more like a guided conversation, turning your day-to-day experiences into clear data your healthcare team can work with. The most important thing? Just be honest.
The whole system is built on a simple idea: assigning a number to how severe each symptom feels. Most common scales, like the Post-Concussion Symptom Scale (PCSS), use a 0 to 6 rating.
It’s pretty intuitive: 0 means you don’t have the symptom at all, while a 6 means it’s severe and really getting in the way of your life. All you have to do is read each listed symptom and circle the number that best matches your experience over a set period, like the past 24 hours.
A Practical Example with Alex
Let’s make this real. Imagine a patient named Alex, who is filling out a questionnaire one week after a minor fall. Alex goes down the list, thinking carefully about each symptom.
Headache: Alex has had a constant, dull ache that seems to crank up in the afternoons. That feels like a 4 (Moderate).
Dizziness: This only happens when Alex gets up too fast. It’s noticeable but doesn’t cause a stumble, so they mark it as a 2 (Mild).
Difficulty Concentrating: Alex describes a persistent "brain fog" that makes it tough to follow along in work meetings. This is a big disruption, so it gets a 5 (Moderate-Severe).
Sadness: There’s been a bit of a low mood, but it’s not overwhelming. Alex decides on a 1 (Very Mild).
After Alex has rated all 22 symptoms on the form, it’s time to find the total symptom score. It's just simple addition—summing up the individual ratings. From these four symptoms alone, Alex's partial score is 12 (4 + 2 + 5 + 1). The final number, after adding all 22 ratings, provides a single, powerful snapshot of their overall symptom burden.
To give you a clearer picture of how this works, here's a sample scoring table.
Example Scoring for a Post-Concussion Symptom Scale (PCSS)
This table illustrates how individual symptom ratings are used to calculate a total symptom score for a hypothetical patient.
Symptom | Patient Rating (0-6 Scale) | Clinical Note |
|---|---|---|
Headache | 4 | Patient reports a persistent, dull ache. |
Dizziness | 2 | Occurs mainly with changes in position. |
Nausea | 0 | Patient reports no feelings of nausea. |
Difficulty Concentrating | 5 | Described as significant "brain fog." |
Sadness | 1 | A very mild, occasional low mood. |
Partial Total Score | 12 | Calculated by adding all rated symptoms. |
As you can see, the final score gives clinicians a quantitative measure to track, rather than relying solely on subjective descriptions.
The Power of a Baseline Score
For athletes or anyone in a high-risk field, the concept of a "baseline test" is a game-changer in concussion management. This is simply a post-concussion symptom questionnaire that's completed before an injury ever happens. It captures what's normal for that person when they are healthy.
A baseline score provides a personalized benchmark. When a concussion is suspected, a new score can be directly compared to the pre-injury baseline, making it much easier for clinicians to identify the true impact of the injury.
This comparison takes the guesswork out of the equation. It allows for a far more precise and personalized recovery plan. Even if you don't have a baseline score, the principle is the same. Tracking your scores over time creates a trendline that maps your recovery. The goal is always to see that total score come down, eventually returning to zero or your personal baseline.
Curious about how these scores translate into a concrete recovery strategy? Contact the Orange Neurosciences team to see how we integrate this crucial data into personalized care plans and help you take the next step.
Turning Your Scores into a Recovery Action Plan
Getting a total score from a post-concussion questionnaire can feel like a final grade, but that single number is really just a snapshot in time. The real magic isn't in one isolated score; it's in watching the trend unfold over several weeks.
Think of it like tracking your fitness. One workout doesn’t tell you much, but logging your performance over a month reveals clear patterns. You can see your strength growing and your endurance improving. In the same way, your symptom scores create a living roadmap of your brain's healing journey.
When you track your symptoms consistently, the questionnaire stops being a simple form and becomes a powerful communication tool. It ensures your treatment plan can evolve right alongside your needs, instead of staying stuck in the past.
From Data to Decisions
The whole point is to turn these numbers into real, actionable insights. Your healthcare provider won’t just look at the total score. They'll dive deeper, analyzing which specific symptom clusters are flaring up. This detailed view is what allows for precise, targeted tweaks to your recovery plan.
Here are a few practical examples of how this plays out:
Physical Symptom Spikes: Let's say your scores for "dizziness" and "balance problems" suddenly jump after you try a new rehab exercise. That's not a failure; it's valuable data. Actionable Insight: Tell your physiotherapist immediately. They can scale the activity back to a level that challenges you just enough to heal, without causing a setback.
Persistent Emotional Scores: If your ratings for "sadness" or "anxiety" stay high—or even creep up—over several weeks, that’s a clear signal. Actionable Insight: Bring this pattern up with your doctor. This might prompt them to recommend specific cognitive therapies or suggest a referral to a psychologist who specializes in the emotional side of injury recovery.
Cognitive Score Plateaus: What if your "difficulty concentrating" score is stuck at a moderate level and just isn't budging? Actionable Insight: Use this data to advocate for your needs. Your team might introduce specific cognitive exercises or recommend assistive technologies to help you manage mental fatigue at work or school.
The questionnaire creates a feedback loop. Your symptoms guide the therapy, and the therapy's effectiveness is measured by your next set of scores. It’s a responsive, collaborative process that puts you at the centre.
This symptom-tracking approach isn't just a good idea; it's becoming a cornerstone of modern concussion care. A landmark Canadian study using the 2020 Canadian Community Health Survey provided the first national estimates on concussion recovery by asking people exactly how long their symptoms lasted. This kind of large-scale insight highlights just how valuable standardized symptom tracking is.
You can dive into the findings of this important Canadian concussion recovery study on StatCan to learn more about the national picture.
Ultimately, your post-concussion symptom questionnaire empowers you to be an active, informed participant in your own recovery. By consistently and honestly sharing your experience, you provide the critical data needed to fine-tune your path back to feeling like yourself again.
Pairing Questionnaires with Digital Recovery Tools
A post-concussion symptom questionnaire is a powerful tool. It gives us a vital, first-person account of your recovery journey. But what if you could pair that personal narrative with objective, real-time data about how your brain is actually performing?
This is where the magic happens. When we bring together traditional self-reporting and modern digital health platforms, we start to see a much more complete picture of the healing process.
Think of it this way: your questionnaire is like telling a mechanic that your car feels sluggish and isn't running right. A digital cognitive tool is like the mechanic plugging in a diagnostic computer to see exactly what's happening under the hood—checking reaction times, processing speed, and cognitive efficiency. Combining both gives you a full, 360-degree view.
Fusing Subjective Feelings with Objective Data
Digital recovery platforms, like the one we've developed at Orange Neurosciences, use engaging, game-based exercises to measure specific cognitive functions. This isn't just about playing games; it's about creating a direct link between what you feel and what your brain can verifiably do.
Let's say on your questionnaire, you rate your "mental fog" as a 5 out of 6. That's a strong feeling, but it's hard to measure. A digital assessment, however, can show us the real-world impact of that fog.
Attention Tasks: It might reveal a 20% decrease in your ability to hold focus compared to your pre-injury baseline.
Reaction Time Tests: It could show that your processing speed is measurably slower, especially when tasks get more complex.
Memory Games: It can pinpoint specific challenges, like a hiccup in short-term recall that lines up perfectly with your self-reported fogginess.
Suddenly, a general feeling is transformed into a specific, measurable target for therapy.
Instead of just knowing you feel fatigued, you can see precisely how that fatigue impacts your cognitive endurance. This allows your care team to design exercises that build stamina at a pace that's challenging but not overwhelming, leading to a much more precise and personalized therapy plan.
The screenshot below shows how a platform like Orange Neurosciences makes complex cognitive data accessible and easy to understand for both clinicians and their patients.

This kind of visual feedback makes it so much easier to track your progress and see the direct results of your therapeutic efforts over time.
Creating a Smarter Recovery Journey
Integrating these digital platforms also makes the entire recovery process more engaging and easier to stick with. Of course, it's critical to consider the importance of cognitive accessibility in digital tools, ensuring they are designed for users who might be dealing with the very cognitive challenges the tools are meant to help.
Well-designed platforms present data clearly, use gamified elements to keep you motivated, and can be used right from the comfort of your home. This data-driven approach takes the guesswork out of recovery. By pairing the rich, personal insights from your post-concussion symptom questionnaire with the hard data from digital assessments, you and your care team can build a truly responsive and effective action plan.
To see how these innovative tools can be woven into your recovery, learn more about Orange Neurosciences' solution and discover how we're helping to create smarter paths to healing.
Frequently Asked Questions About Concussion Questionnaires
Navigating concussion recovery can feel overwhelming, and it’s completely normal to have a lot of questions. A post-concussion symptom questionnaire is one of the most important tools in your toolkit, but knowing how to use it right makes all the difference.
Let's walk through some of the most common questions we hear from patients and families to give you some clear, practical answers.
How Often Should I Complete a Questionnaire?
There’s no single answer here—it really comes down to where you are in your recovery and what your doctor recommends.
Right after an injury, in the acute phase, you might be asked to fill one out daily, or at least every few days. This gives your care team a really detailed, day-by-day snapshot of what’s going on as your symptoms evolve.
As you start to feel better and things stabilize, that frequency might drop to once a week or every two weeks. For athletes in a return-to-play protocol, it's often a requirement before and after every new stage of activity. This is crucial for making sure you aren't pushing your brain too hard, too soon. A practical example: a soccer player might fill one out on Tuesday, do a light, non-contact drill on Wednesday, and then fill out another on Thursday to see if the activity caused any symptoms to spike.
The key isn't a single score on a single day. The real power of a post-concussion symptom questionnaire comes from the trends it shows over time. Consistency is everything—it’s this data that allows your provider to make the best decisions for your care.
Can I Fill Out the Questionnaire on My Own?
Absolutely. In fact, you should. These questionnaires are designed to be self-reported, meaning you fill them out based on your own experience.
Doing this in the comfort of your own home, without the pressure of a doctor's office, often leads to a more accurate picture of your symptoms. It's easy to forget things when you're on the spot.
But here’s the important part: while you can fill it out on your own, you shouldn't interpret it on your own. Think of yourself as the detective gathering the clues, and your healthcare provider as the expert who analyzes them. Any changes to your treatment plan must be made in collaboration with a professional.
For instance, if you notice your headache score suddenly shoots up after you start a new exercise, your actionable next step is to call your doctor. Don't just stop the exercise and hope for the best; share the data so they can adjust your plan properly.
What if My Symptom Scores Are Not Improving?
Seeing your scores hit a plateau—or worse, start to climb—is a clear sign that you need to reach out to your healthcare provider right away.
This is precisely why tracking your symptoms is so valuable. It gives you concrete, objective proof when your recovery has stalled or is heading in the wrong direction.
This is not a sign that you’ve failed. Not at all. It's a vital signal that your current recovery plan needs a tweak. Your care team might look into different therapies, suggest more tests, or explore other factors that could be getting in the way of your progress.
One of the most common culprits holding back recovery is poor sleep. A lack of quality sleep can amplify nearly every concussion symptom, from headaches to brain fog. To dig deeper into this, you can learn more about how concussions can impact sleep patterns. The bottom line? Never ignore worsening scores. They’re your body’s call to action.
Ready to move beyond just tracking symptoms and get an objective look at your brain's recovery? The innovative tools from Orange Neurosciences combine your personal feedback with precise cognitive data, creating a therapy plan that's truly built for you. Contact us today or check out our solutions to learn more.

Orange Neurosciences' Cognitive Skills Assessments (CSA) are intended as an aid for assessing the cognitive well-being of an individual. In a clinical setting, the CSA results (when interpreted by a qualified healthcare provider) may be used as an aid in determining whether further cognitive evaluation is needed. Orange Neurosciences' brain training programs are designed to promote and encourage overall cognitive health. Orange Neurosciences does not offer any medical diagnosis or treatment of any medical disease or condition. Orange Neurosciences products may also be used for research purposes for any range of cognition-related assessments. If used for research purposes, all use of the product must comply with the appropriate human subjects' procedures as they exist within the researcher's institution and will be the researcher's responsibility. All such human subject protections shall be under the provisions of all applicable sections of the Code of Federal Regulations.
© 2025 by Orange Neurosciences Corporation



