A Proactive Guide to Preventive Medical Care for Brain Health
Jan 4, 2026
Preventive medical care is all about getting ahead of health issues. Instead of waiting for symptoms to show up and then scrambling for a treatment, this approach focuses on preventing disease before it even starts. It’s a combination of proactive screenings, smart lifestyle choices, and early interventions designed to keep you well for the long haul—especially when it comes to your cognitive health. For example, instead of waiting for memory loss to become a daily problem, preventive care helps you track your cognitive baseline early on so you can make small, effective changes to diet or exercise at the first sign of a shift.
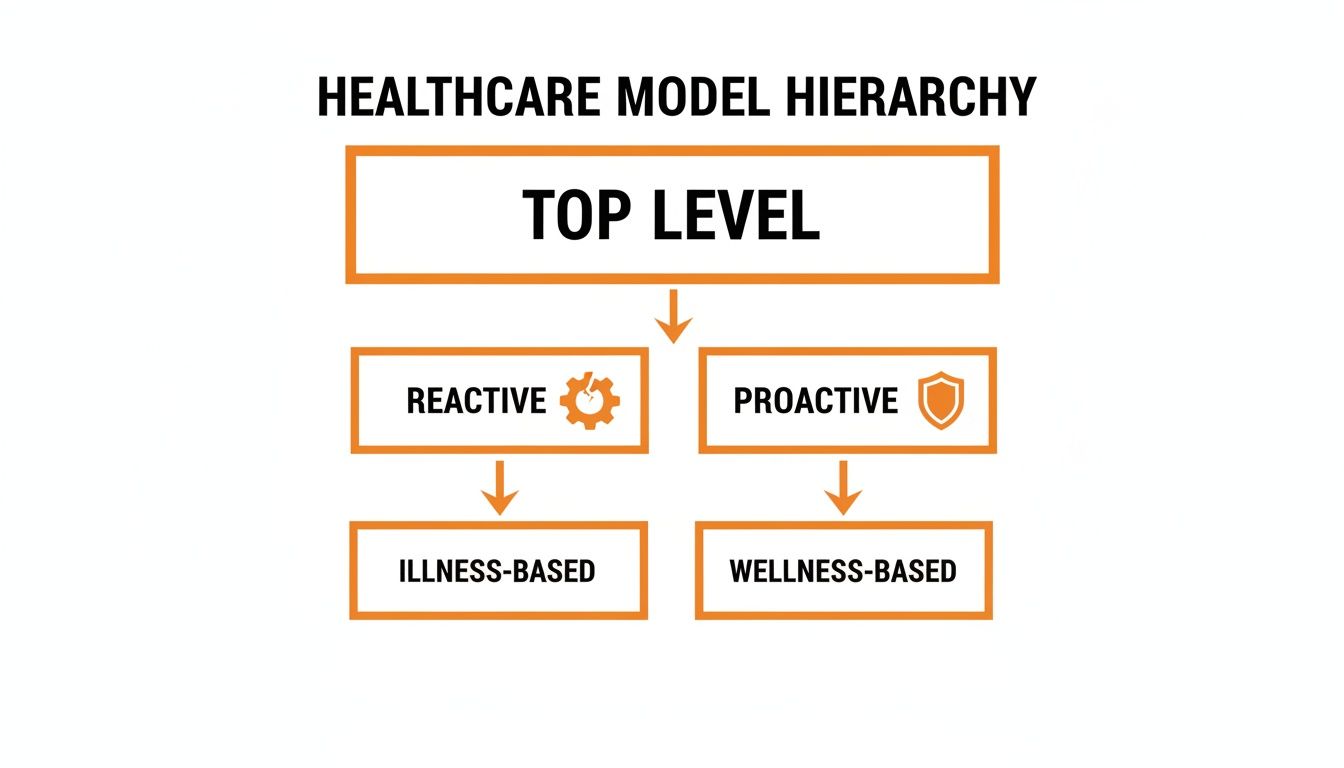
Shifting Healthcare from Reaction to Prevention
For as long as most of us can remember, medicine has worked on a reactive basis. You feel sick, you go to the doctor, you get a diagnosis, and you start a treatment. This "break-fix" model is absolutely critical for acute problems, but it completely misses the boat on conditions that creep up on us slowly over many years.
Think of it like taking care of your car. You wouldn't just keep driving until the engine seizes before you finally decide to get an oil change, right? Of course not. You follow a regular maintenance schedule to keep it running smoothly and avoid a total breakdown. Preventive care applies that exact same logic to our most important asset: our bodies and brains.
This isn't just about getting your annual physical. It's a fundamental change in how we think about health—moving from just treating illness to actively building wellness.
The Proactive Wellness Model
A proactive approach is all about spotting potential risks early and making small, consistent changes that pay huge dividends down the road. This is especially true for brain health, where tiny, almost unnoticeable changes can be the very first signs of future problems. The goal is to create a continuous cycle of care that involves:
Early and Regular Screenings: By establishing a baseline for both physical and cognitive health, doctors can track how you're doing over time. This makes it much easier to spot any deviations from your personal norm long before they become a serious issue. Actionable Insight: Schedule a baseline cognitive assessment during your next annual physical to create a benchmark for future comparison.
Personalised Lifestyle Adjustments: Based on what your screenings show and other risk factors, you can make specific, targeted changes to your diet, exercise routine, and sleep habits to better protect your health. For example, if a screening shows a slight dip in processing speed, your doctor might suggest incorporating brain-healthy foods like salmon and blueberries into your diet.
Targeted Early Interventions: When a potential issue is flagged early on, the interventions are often far more effective and much less invasive. The result? Dramatically better health outcomes.
This shift empowers everyone involved. For families, it offers a real, tangible way to protect their future well-being. For the healthcare system as a whole, it means better patient outcomes and a massive reduction in the costs of managing chronic diseases.
You can take a leading role in this new model, too. To truly move from being reactive to proactive, you can start by building an action plan for longevity through at-home health testing and gaining insights into your own health future.
Embracing this proactive mindset means we're no longer passive bystanders in our own health journeys. It's about creating a true partnership between you and your healthcare provider, powered by modern tools that make consistent monitoring simple and actionable. To see how technology is making this happen, you can explore the workflow of modern preventive tools. By putting prevention first, we’re not just treating today’s problems—we’re investing in a healthier, more resilient future.
The Four Pillars of Preventive Medical Care
To really get a handle on preventive medical care, it helps to think of it not as one single action, but as a strategy with four distinct levels. Each one—what we call a pillar—is a chance to step in, protect a person's health, and improve their long-term well-being. When you put them all together, they create a complete game plan for staying healthy, especially when it comes to something as vital as cognitive health.
The big idea here is a fundamental shift in thinking: moving away from a reactive, illness-focused model to a proactive, wellness-based one.
This proactive approach means we tackle health challenges upstream, long before they snowball into critical and costly problems.
Understanding the Four Levels of Preventive Care
To see how these pillars work in the real world, let's break them down. Each level targets a different audience with a different goal, from broad public health initiatives to highly personalized care for individuals already managing a condition. The following table maps out what each level aims to achieve.
Level of Prevention | Main Goal | Target Audience | Practical Example (General Health) | Practical Example (Cognitive Health) |
|---|---|---|---|---|
Primordial | To stop risk factors from even emerging. | Entire populations, communities. | Creating safe city parks to encourage physical activity. | Public campaigns promoting early childhood nutrition for brain development. |
Primary | To prevent a specific disease before it starts. | Individuals or groups at risk of a specific condition. | Getting vaccinated against the flu. | Promoting mentally stimulating hobbies like learning a language to build cognitive reserve. |
Secondary | To detect a disease at its earliest stage. | Individuals who may have an undiagnosed condition. | Routine blood pressure screenings to catch hypertension early. | Regular brain health assessments to detect subtle changes in memory or attention. |
Tertiary | To manage an existing condition and prevent complications. | Individuals with a diagnosed disease or condition. | Cardiac rehab for a patient who has had a heart attack. | Targeted cognitive training to help someone with mild impairment maintain daily function. |
As you can see, these pillars create a complete safety net, offering support at every possible point in a person's health journey.
Pillar 1: Primordial Prevention
The very first level, primordial prevention, is about stopping risk factors from ever developing in the first place. It’s the most upstream approach, targeting the broad social and environmental conditions that can eventually lead to poor health.
Think of it like building a safe community playground. You’re not there to treat scraped knees; you’re installing soft surfaces and well-maintained equipment to create an environment where those injuries are far less likely to happen at all.
For brain health, this might look like a public health policy that ensures widespread access to nutritious food for children, setting up a foundation of wellness for an entire generation.
Pillar 2: Primary Prevention
Next up is primary prevention. This is where we take direct action to prevent a specific disease or injury before it can take hold. For most people, this is what comes to mind when they hear the term "preventive care."
Here are a few classic examples:
Vaccinations: Getting immunised against diseases like measles or polio is primary prevention in action.
Healthy Lifestyle Choices: Encouraging people to exercise regularly and eat a balanced diet to prevent conditions like heart disease or type 2 diabetes. Actionable Insight: Commit to a 30-minute walk each day and swap one processed snack for a piece of fruit to actively lower your risk of chronic disease.
Cognitive Stimulation: On the brain health front, this could mean promoting lifelong learning or engaging in puzzles and games that challenge the mind, effectively building up its resilience.
This stage is all about actively defending yourself and your community from known health threats.
Pillar 3: Secondary Prevention
Secondary prevention is all about early detection. The goal here is to find and treat a disease at its earliest, most manageable stage—often before a person even notices any significant symptoms. This is where regular screenings become absolutely essential.
The core idea of secondary prevention is simple: you can't manage what you don't measure. By catching problems early, we dramatically improve the chances of a successful outcome.
Things like routine mammograms for breast cancer or blood pressure checks for hypertension are perfect examples. In the world of cognitive health, this is where regular brain health screenings play a powerful role. They can establish a personal baseline and flag subtle changes in memory or attention years before they might otherwise become obvious.
Pillar 4: Tertiary Prevention
Finally, we have tertiary prevention. This level focuses on managing an existing health condition to stop it from getting worse or causing other complications. The disease is already there, but the goal is to soften its impact and improve a person's quality of life.
For instance, someone who has had a heart attack might join a cardiac rehabilitation program to regain strength and prevent a future event. In a similar vein, an individual diagnosed with early cognitive impairment might use targeted cognitive training programs to help maintain their independence and daily function for as long as possible.
These four pillars aren’t separate silos; they are deeply connected parts of a lifelong health strategy. A truly effective healthcare system weaves all four together, ensuring the right support is available at every stage. This holistic view is critical for creating a strong continuity of care plan for patients, especially when it comes to managing something as complex as long-term cognitive wellness.
Why Early Cognitive Screening Is Non-Negotiable
We’re meticulous about tracking blood pressure and cholesterol for our hearts. We get it—early warnings mean we can act fast. But what about our brain, the very centre of who we are? All too often, we wait for serious, life-altering problems to show up before we even think about its health. This reactive approach is a massive missed opportunity. The truth is, subtle shifts in memory, attention, or decision-making can be the earliest whispers of an underlying issue.

Treating brain health as a core part of preventive medical care is just about applying the same logic we use for physical health. Regular, early screening isn't about looking for a diagnosis to worry about. It’s about establishing your personal baseline—what’s normal for you—so you can spot meaningful changes if they ever appear.
Establishing a Lifelong Cognitive Baseline
Just like we have recommended schedules for physicals, a proactive approach to brain health should follow us through life’s key stages. This isn't a one-and-done test; it’s a continuous conversation with your own health that provides invaluable insights over a lifetime.
For Children and Adolescents: Cognitive screening in schools can be a real game-changer. It helps educators and parents track crucial developmental milestones in attention, memory, and processing speed. Catching challenges early on can lead to targeted support that doesn't just improve academic performance but sets a foundation for long-term success. Practical Example: A school might use a screening tool to identify a 3rd grader's attention difficulties, leading to a simple classroom accommodation like preferential seating that dramatically improves their learning.
For Adults in Mid-Life (40s-50s): This is the sweet spot for establishing a firm cognitive baseline. Think of it like taking a high-resolution snapshot of your brain's current performance. This baseline becomes the all-important reference point for any future check-ins, making it so much easier to detect real changes down the road.
For Older Adults (60s and Beyond): Here, regular follow-up screenings become vital for keeping an eye on cognitive function. These assessments can help tell the difference between normal, age-related memory slips (we all have them!) and more concerning patterns that might need a closer look from a specialist.
The most damaging myth in cognitive health is that significant decline is just an inevitable part of getting older. The evidence shows the opposite: early detection and intervention can dramatically alter health trajectories, preserving independence and quality of life for years to come.
By making regular screenings a normal part of our health routine, we shift cognitive health from a source of anxiety to a manageable part of our overall wellness plan. If you're curious about what this actually looks like, our guide on taking a cognitive screening test online walks you through how modern tools have made the process straightforward and accessible.
Identifying Who Benefits Most from Screening
While everyone can benefit from knowing their cognitive baseline, some people should absolutely prioritise it. It's the same principle as someone with a family history of heart disease being more vigilant about their cardiovascular health. Certain risk factors for cognitive decline simply call for a more focused approach.
These factors can help determine risk and guide how often screenings should happen:
Family History: Having a close relative with dementia or another neurodegenerative condition significantly increases personal risk.
Chronic Health Conditions: Things like cardiovascular disease, diabetes, and hypertension are all closely tied to brain health. Managing these conditions is a powerful form of preventive medical care for the brain.
Lifestyle Factors: A history of smoking, a sedentary lifestyle, or consistently poor nutrition can all take a toll on long-term cognitive function.
History of Head Trauma: Even a single significant concussion can have lasting effects that are important to monitor over time.
For anyone with one or more of these risk factors, starting a regular screening schedule earlier in life is one of the smartest health decisions you can make.
Moving from Guesswork to Actionable Data
Ultimately, early cognitive screening is about empowerment. It replaces that vague fear of the unknown with clear, objective data that you and your doctor can actually work with.
For example, a screening might show a subtle dip in your processing speed. Instead of waiting for that to become a noticeable, daily frustration, your healthcare provider can suggest targeted interventions. This could be anything from specific brain-training exercises and dietary adjustments to a new physical activity routine. This proactive stance is the very heart of effective preventive medical care.
By embracing early screening, we’re not just sitting around waiting for a storm to hit. We're actively checking the forecast, reinforcing the foundations, and making sure we're ready for whatever comes our way. It’s time our brains got the same thoughtful, proactive care we’ve long given the rest of our bodies.
Overcoming Barriers to Preventive Care in California
Everyone agrees that preventive medical care is a good thing, but making it happen in the real world is another story entirely. It's one thing to talk about proactive health; it's another to actually get it. Let's use California as a real-world example to look at the roadblocks—from not having enough doctors to massive gaps in access—and, more importantly, focus on the practical solutions that are working right now.
Getting care, even when you know you need it, can be a struggle. In California, primary care is supposed to be the backbone of preventive medical care, but the state is facing a serious shortage. As of 2022, there was only one primary care physician for every 1,199 people. Looking ahead, the state will need another 10,500 primary care providers by 2030 just to keep up.
This problem hits hardest in rural communities, where about 7 million Californians live in areas officially designated as health professional shortage areas. This isn't just an inconvenience; it means longer waits, delayed care, and worse health outcomes. You can get a clearer picture of this challenge by reading about California's efforts to increase access to healthcare providers.
This gap sends ripples through the whole system, making it tougher for people to get the screenings and early support they need. But this isn't an impossible problem. It just means we need to get smarter and more efficient about how we deliver care.
Integrating Scalable Solutions in Clinical Settings
For a busy clinic, the thought of adding one more screening to an already jam-packed schedule sounds like a nightmare. The trick isn't to pile on more work, but to bring in tools that make the existing workflow smoother and more impactful. This is exactly where fast, scalable digital assessments can be a game-changer.
Think about a primary care clinic wanting to add baseline cognitive screenings for its patients over 40. The old way would be referring every patient to a specialist, a process that can drag on for months. Instead, they could use a tool that provides an objective cognitive profile in less than 30 minutes, right there during a routine check-up.
This simple change brings huge benefits right away:
Efficiency: It makes screening straightforward, letting clinics see more patients without burning out their staff or creating long waitlists.
Actionable Data: Doctors get clear, easy-to-read data instantly, helping them decide on the spot if a specialist follow-up is truly needed.
Reduced Patient Burden: Patients get real insights into their brain health without the stress and delay of bouncing between appointments.
By weaving these efficient tools directly into their existing routines, clinics can shift preventive care from being an extra task to a core, manageable part of every patient's health journey.
Leveraging Schools to Bridge Community Gaps
Another powerful approach is to bring preventive medical care to where people already are. For kids, that’s school. School-based health centres (SBHCs) are becoming lifelines, especially in rural and underserved areas where seeing a pediatric specialist is next to impossible.
These centres can use digital assessment tools to help teachers spot students who might need early support for learning or developmental challenges. For instance, a school could roll out a screening program for attention or memory issues that could be holding a student back in class.
This strategy helps in a few critical ways:
Early Identification: It catches potential issues when interventions are most likely to make a real difference.
Reduces Stigma: When cognitive health check-ups are just a normal part of the school year, the stigma around learning challenges starts to fade away.
Improves Equity: It gives every child a fair shot at early screening and support, no matter their family’s ability to access specialized medical care.
This model is a perfect example of how new thinking can help healthcare providers deliver preventive care more effectively and reach kids who have been overlooked for too long.
Driving Policy with Long-Term Value
At the end of the day, getting preventive cognitive services widely adopted comes down to proving their long-term value. When policymakers and insurance companies see hard evidence that early screenings save a fortune down the road—by preventing the need for expensive treatments for advanced conditions—the whole system starts to change.
This data-first approach is already starting to shape policy. By demonstrating how proactive care leads to better outcomes and lower costs across the board, we create a strong incentive for insurance plans to cover these essential services. This is how proactive brain health stops being just a nice idea and becomes a financially smart, essential part of modern healthcare.
How AI Is Changing the Game in Brain Health Screening
For years, getting a clear picture of someone's cognitive health was a slow, often subjective process. This created a major roadblock for proactive preventive medical care, leaving families and healthcare providers looking for a faster, more objective way to get real answers. Thankfully, artificial intelligence is stepping in to fill that exact gap. It's taking brain health screening from a complex, specialist-only procedure and turning it into something scalable and accessible for routine check-ups.
AI-powered platforms are taking the mystery out of cognitive health by giving us a clear, data-driven look at how the brain is functioning. Instead of just relying on observations or long, drawn-out questionnaires, these systems use smart algorithms to analyze how a person performs in key cognitive areas.
What does this mean in practice? It means we can generate a detailed, objective profile of someone's memory, attention, and executive function in as little as 30 minutes. That kind of speed and precision takes the guesswork out of the equation, which has held back early detection for far too long.

This image really captures the essence of modern screening—it’s a portable, efficient tool that slots sophisticated assessments right into the daily clinical workflow.
Turning Data Into Actionable Insights
The real magic of AI here isn't just about collecting data; it's about making that data useful right away. These platforms give clinicians real-time reports that are easy to understand, flagging any subtle changes from a person's own baseline or from age-appropriate norms. This makes informed, on-the-spot decisions possible.
If you're curious about how technology is making waves in other areas of health, it's worth reading a cardiologist’s perspective on the smartwatch ECG to see the parallels in proactive health management.
Think about it: instead of waiting months for a specialist referral, a family doctor can use AI-driven insights to figure out the next steps immediately. That might mean recommending specific lifestyle adjustments, starting targeted cognitive exercises, or making a much more informed referral for a deeper evaluation. It empowers providers to deliver truly personalized care at a scale we couldn't before.
The core benefit of AI-powered screening is its ability to translate complex cognitive performance into a clear, actionable roadmap. It bridges the gap between an initial concern and an effective intervention, making proactive care a practical reality for clinics of all sizes.
Making Screening Engaging and Effective for Everyone
One of the biggest hurdles in cognitive assessment, especially with kids and older adults, is keeping them engaged. Let's be honest, traditional tests can be boring, intimidating, or just plain stressful, which can skew the results. AI-driven platforms are tackling this head-on by using gamified assessments.
Tools like OrangeCheck and ReadON embed sophisticated cognitive tests into fun, game-like interfaces. This simple shift makes the whole process feel less like a test and more like a puzzle or a challenge.
For Children: Gamified tasks can check attention and processing speed without causing frustration, giving a much more accurate snapshot of a child's developmental journey.
For Adults: An engaging format helps lower any test-related anxiety, which leads to more reliable baseline data and makes it easier to track cognitive changes over time.
This user-friendly design doesn't just produce better data; it also encourages people to stick with follow-up screenings, which is crucial for effective long-term monitoring. By making the experience a positive one, these tools help normalize the whole idea of a regular brain health check-up.
Empowering Providers to Bridge Care Gaps
At the end of the day, AI is what's making comprehensive preventive medical care for brain health truly achievable. By offering objective, quick, and scalable screening solutions, this technology gives providers the power to make better-informed decisions and proactively manage their patients' health. It hands them the tools they need to spot risks early, personalize what they recommend, and track outcomes with real precision.
These platforms aren't just another piece of tech; they represent a fundamental shift in how we approach cognitive wellness. To see how these tools fit into a complete system for proactive health, learn more about our solution for cognitive assessment and therapy. By breaking down the old barriers, AI is clearing the path for a future where brain health is a priority in every check-up, for every single patient.
Measuring Success and Taking Your Next Step
So, how do we know if a proactive approach to preventive medical care is actually making a difference? When it comes to cognitive health, success is so much more than just avoiding a diagnosis. It's about seeing real, tangible improvements in day-to-day life.
Think about a student who can suddenly focus better in class, an employee whose performance sharpens at work, or an older parent who maintains their ability to live independently. That’s what success looks like.
True success isn't a one-off test result. It's a story told through data points collected over time, showing a positive trend. This ongoing tracking creates a powerful feedback loop, letting families and healthcare providers see the incredible value of stepping in early and staying consistent.
Defining What Success Looks Like
The trick is to track objective metrics that actually mean something in the real world. Instead of just asking, "How's your memory holding up?" a data-driven approach measures specific cognitive skills.
Meaningful metrics might include:
Improved Processing Speed: Tasks that used to feel like wading through mud now feel quicker and more automatic. Practical Example: A patient notices they can follow conversations in a noisy restaurant more easily after three months of targeted brain exercises.
Enhanced Attention and Focus: Someone can stay locked in for longer, whether it’s during a work meeting or while tackling homework.
Stable Executive Function: Core skills like planning, organising, and problem-solving stay sharp and effective.
Maintained Quality of Life: This is the big one. It’s about a person continuing to enjoy their hobbies, social life, and daily routines with confidence.
When we track these concrete data points, the benefits of preventive care become clear and undeniable. The conversation shifts from a place of fearing a potential diagnosis to feeling empowered by measurable progress.
A Path Forward Driven by Data
This data-first mindset is becoming a real cornerstone of public health policy. Just look at California's CalAIM initiative. It has set a bold goal for 2025: ensuring all Medi-Cal managed care plans score above the 50th percentile on every single preventive care measure for children.
A huge part of this is boosting developmental screenings to catch neurodevelopmental issues as early as possible. To hit this target, they need tools that can provide objective profiles in areas like attention and memory, which helps personalise support and track progress effectively. You can learn more about California’s ambitious public health goals here.
This move signals a much bigger trend: we’re starting to use objective data not just to treat sickness, but to build a foundation of lasting wellness for entire communities.
Take Your Next Step Toward Proactive Care
Adopting a strategy of proactive preventive medical care is one of the most powerful investments you can make in your long-term health. By focusing on early screening, establishing a personal baseline, and consistently monitoring cognitive function, you replace guesswork and anxiety with clear, actionable information.
This approach puts you back in the driver’s seat, empowering you to make informed decisions that protect your brain health for years to come.
If you’re ready to bring a modern, data-driven strategy for cognitive wellness into your clinic, school, or family, the best next step is to see how these tools work firsthand. We encourage you to visit the Orange Neurosciences website to request a demo and discover how our platform can make proactive brain health a practical reality for you.
Your Questions About Preventive Care, Answered
Stepping into the world of preventive medical care, especially when it comes to brain health, naturally brings up a few questions. Let's walk through some of the common ones to help you see how you can put these strategies into practice for your family.
How Often Should My Family Get a Cognitive Screening?
The best answer is: it depends on your age and your unique risk factors. It helps to think of a cognitive screening less like a one-time test and more like a regular dental cleaning—a consistent check-in to stay on top of your health.
For Children: The key is to align screenings with major developmental milestones. This allows us to track how crucial skills like attention and memory are progressing over time.
For Adults: A great goal is to establish a personal cognitive baseline sometime in your 40s or 50s. From there, a check-in every 2-5 years is a good rule of thumb, unless you or your doctor notice any changes that warrant an earlier look.
For Those at Higher Risk: If you have a family history of dementia or other risk factors like hypertension, it’s smart to chat with your doctor. Together, you can create a more personalized and frequent screening schedule that makes sense for you.
Thanks to modern digital tools, these check-ins are now quick and easy, fitting smoothly into a routine doctor’s visit without feeling like a major ordeal.
Is Preventive Cognitive Screening Covered by Insurance?
This is a big question, and an important one. The good news is that coverage for preventive cognitive screenings is getting better all the time. The healthcare system is finally starting to recognise just how much money can be saved in the long run by catching potential issues early.
While the specifics will always vary between insurance plans here in Canada, many healthcare providers are starting to build these assessments right into standard wellness visits. The best first step is always to talk directly with your clinic and your insurance provider about your options.
A core part of our mission at Orange Neurosciences is to create affordable and accessible solutions that open the door to this vital service for everyone, no matter their coverage.
What's the Difference Between an AI Screening and a Full Neuropsychological Exam?
This is a fantastic question because it gets to the heart of what makes proactive screening so powerful. Here’s a simple way to think about it: an AI-powered screening is like a blood pressure cuff for your brain.
It’s a quick, objective tool designed to be used widely and easily, whether in a doctor's office or a school. The whole point is to get a fast, reliable snapshot of cognitive functions—like memory and attention—to see if there’s any reason to take a deeper look.
A full neuropsychological exam is that deeper look. It's a much more comprehensive, diagnostic evaluation that a specialist would order, but only after an initial screening flags a potential concern.
The AI screening is what makes proactive preventive medical care possible on a large scale. The traditional exam is the specialized diagnostic tool we use when it's truly needed.
Ready to take the next step in proactive brain health? Orange Neurosciences provides the tools to make data-driven cognitive care a reality for your clinic, school, or family. Visit our website to request a demo and see how our platform can support your preventive care goals.

Orange Neurosciences' Cognitive Skills Assessments (CSA) are intended as an aid for assessing the cognitive well-being of an individual. In a clinical setting, the CSA results (when interpreted by a qualified healthcare provider) may be used as an aid in determining whether further cognitive evaluation is needed. Orange Neurosciences' brain training programs are designed to promote and encourage overall cognitive health. Orange Neurosciences does not offer any medical diagnosis or treatment of any medical disease or condition. Orange Neurosciences products may also be used for research purposes for any range of cognition-related assessments. If used for research purposes, all use of the product must comply with the appropriate human subjects' procedures as they exist within the researcher's institution and will be the researcher's responsibility. All such human subject protections shall be under the provisions of all applicable sections of the Code of Federal Regulations.
© 2025 by Orange Neurosciences Corporation



