MoCA vs MMSE Choosing the Right Cognitive Screen
Dec 9, 2025
When you're standing at a clinical crossroads, trying to decide between the MoCA and the MMSE, the fundamental difference comes down to one word: sensitivity.
Simply put, the MoCA is vastly better at picking up on Mild Cognitive Impairment (MCI). The MMSE, on the other hand, has its place as a long-standing tool for tracking the progression of moderate to severe dementia. This makes the Montreal Cognitive Assessment (MoCA) the go-to screener for early detection, especially when dealing with patients who have subtle symptoms or a higher level of education that might mask initial deficits.
A Clinician's Quick Guide to MoCA vs MMSE
Choosing the right cognitive screening tool isn't just a box-ticking exercise; it's a critical first step that shapes a patient's entire care pathway. While both the MoCA and the Mini-Mental State Examination (MMSE) are staples in clinics everywhere, they were designed for different jobs. Knowing when to use which is key.
The MMSE, developed way back in 1975, has been a workhorse in cognitive screening for decades. Its main advantages are speed and simplicity, making it a practical choice for a quick check-in with patients who already have noticeable cognitive decline.
But there's a well-known catch: the MMSE has a significant "ceiling effect." This means that people with a high cognitive reserve—like those with more years of education—or those in the very early stages of impairment can easily score in the normal range. That's a huge problem, as it can lead to missed opportunities for crucial early intervention.
This is exactly the gap the MoCA was created to fill in 2005. It deliberately includes more demanding tasks that probe complex areas like executive function and abstract thinking, domains the MMSE barely touches.
Because of this added complexity, the MoCA boasts a much higher sensitivity for MCI—somewhere around 90%. That figure stands in stark contrast to the MMSE's sensitivity for MCI, which is estimated to be as low as 18%.
MoCA vs MMSE: A Side-by-Side Clinical Overview
To see how this plays out in the real world, let's imagine two common clinical scenarios.
First, you have an older adult with a university degree who reports some minor, nagging memory lapses but is otherwise functioning perfectly well. Actionable insight: In this case, the MoCA is the far better choice. It’s designed to catch those nuanced deficits that the MMSE would almost certainly miss.
Now, consider a patient with an established diagnosis of moderate Alzheimer's disease. Your goal is to monitor their decline over time. Actionable insight: Here, the MMSE’s straightforwardness and speed might be all you need to get a reliable snapshot during follow-up visits.
To make the choice even clearer, this table breaks down the essential distinctions between the two screeners.
MoCA vs MMSE A Side-by-Side Clinical Overview
Attribute | Montreal Cognitive Assessment (MoCA) | Mini-Mental State Examination (MMSE) |
|---|---|---|
Primary Use Case | Detecting Mild Cognitive Impairment (MCI) and subtle deficits. | Screening for moderate to severe dementia and tracking decline. |
Administration Time | 10–15 minutes | 5–10 minutes |
Key Domains Tested | Executive function, visuospatial skills, memory, attention, language. | Orientation, registration, recall, language, simple construction. |
Sensitivity for MCI | High (approx. 90%) | Low (approx. 18%) |
Accessibility | Requires mandatory training and certification for clinical use. | Widely known, but proprietary and may involve licensing fees. |
Ultimately, it’s important to remember that tools like the MoCA and MMSE are just the starting point. They are screeners, not diagnostic instruments. They signal that a deeper look is needed.
To see how you can build on these initial findings, it's worth exploring how digital platforms can provide the next layer of insight. You can learn more about the advanced cognitive assessments from Orange Neurosciences that offer a more detailed, longitudinal view of a patient's cognitive health.
Analyzing the Cognitive Domains Each Test Assesses
When you're comparing the MoCA vs. MMSE, it's not just about which one is "harder" or more sensitive. The real story is in what they measure. These two tests probe different areas of cognitive function, and that's precisely why one often catches what the other misses. Understanding this distinction is fundamental to accurate clinical assessment.
The MMSE primarily sticks to a few core areas, making it a relatively quick but narrow snapshot. Its main focus is on orientation (knowing the date and where they are), memory (registering and recalling three words), and some simple language tasks. It’s valuable for spotting more obvious deficits but tends to glide right over the complex, higher-order processes that often show the first signs of trouble in neurodegenerative conditions.
The MoCA, on the other hand, was specifically built to cast a much wider net. It digs into a broader spectrum of cognitive abilities, giving clinicians a more detailed and nuanced picture of a patient's mental functioning.
The MoCA's Comprehensive Cognitive Profile
The Montreal Cognitive Assessment deliberately includes more demanding tasks that evaluate functions the MMSE doesn’t even touch. This thorough approach is what makes it so powerful for detecting the subtle shifts associated with Mild Cognitive Impairment (MCI).
Here are the key domains where the MoCA really shines:
Executive Function: This is the big one. The MoCA directly tests planning, mental flexibility, and abstract thinking. It does this through tasks like the Trail Making Test (connecting numbers and letters in sequence) and verbal abstraction (finding the link between words like "watch" and "ruler").
Visuospatial Skills: The MoCA ups the ante with more complex visuospatial challenges, like drawing a three-dimensional cube and a clock face showing a specific time. These tasks require a much higher level of visual perception and motor planning than the MMSE’s simple figure-copying task.
Memory Recall: Both tests look at memory, but the MoCA’s delayed recall is tougher. It uses five words and gives no hints or category cues, making it a more rigorous test of pure recall compared to the MMSE's three-word task.
Attention and Concentration: The MoCA evaluates attention from multiple angles, including forward and backward digit spans and a vigilance task where the patient taps their hand when they hear a specific letter. This gives you a much better read on their sustained attention.
Language and Verbal Fluency: The MoCA’s language assessment is far more extensive. It includes a verbal fluency task (naming as many words as possible starting with a certain letter in one minute) and more complex sentence repetition. It also uses less common animals for a naming task (e.g., lion, rhino, camel), which can be more revealing.
Actionable Insight: The MoCA is not just a harder version of the MMSE; it's a fundamentally different tool. Use it specifically to probe the cognitive domains—especially executive function—that are critical for the early and accurate detection of MCI.
How These Differences Play Out in Clinical Practice
The practical impact of these different cognitive profiles is huge. Practical Example: Imagine a 68-year-old accountant who comes in feeling "not as sharp" but doesn't have any obvious memory complaints. They could easily score a 28/30 on the MMSE because their orientation and basic recall are perfectly fine.
But when you give them the MoCA, the story changes. They might really struggle with the Trail Making Test, revealing poor mental flexibility. The abstraction task might also trip them up, pointing to a subtle decline in executive function. This is a classic scenario where the MoCA uncovers early deficits that the MMSE would completely miss, triggering a much-needed, deeper workup. For a closer look at assessing these critical skills, our guide on how to test for executive dysfunction offers more detailed insights.
Here’s a practical breakdown of the contrast:
Cognitive Domain | Montreal Cognitive Assessment (MoCA) | Mini-Mental State Examination (MMSE) |
|---|---|---|
Executive Function | Directly assessed via Trail Making, abstraction, and fluency tasks. | Not directly assessed. Offers no insight into planning or mental flexibility. |
Visuospatial Skills | Requires copying a 3D cube and drawing a clock, testing complex planning. | Requires copying intersecting pentagons, a much simpler construction task. |
Memory | Tests delayed recall of five words with no cues. | Tests delayed recall of three words, a less challenging task. |
Attention | Uses multiple tasks, including digit span and a vigilance test. | Uses serial sevens or spelling "world" backward, a single, simpler task. |
This comparison makes it clear why the MoCA vs. MMSE debate really comes down to your diagnostic goal. If you're screening for early, subtle cognitive changes, the MoCA’s broad assessment, particularly of executive function, is indispensable. But if you're just tracking the decline in established, moderate-to-severe dementia, the MMSE’s narrower focus might be enough. The choice always circles back to the clinical question you're trying to answer.
Comparing Diagnostic Sensitivity and Specificity
When you're trying to choose between the MoCA and the MMSE, what it really boils down to is diagnostic accuracy. To make a smart choice that will genuinely impact your patient's outcome, you need to get a handle on two key psychometric properties: sensitivity and specificity.
Simply put, sensitivity is a test's ability to correctly spot someone who has a condition, like Mild Cognitive Impairment (MCI). Specificity, on the other hand, is its ability to correctly identify someone who doesn't have it. A test high in sensitivity is great at catching the condition, while one high in specificity is great at ruling it out.
The MMSE has a well-known and significant flaw: the "ceiling effect." This happens when a test is just too easy for a certain group, leading to scores that look normal but actually hide real, underlying problems.
A patient with a high level of education or a strong cognitive reserve, for example, might sail through the MMSE and score in the normal range, even while experiencing subtle but very real cognitive decline. This is a classic false negative, and it can delay crucial further investigation and care.
The MoCA's Edge in Early Detection
The MoCA was built from the ground up to fix the MMSE's ceiling effect. It includes more complex tasks that really challenge executive function, visuospatial skills, and memory recall. This design effectively lowers the ceiling, making it much more likely to catch impairment in its earliest stages.
This gives the MoCA a much higher sensitivity for MCI. Study after study shows the MoCA's sensitivity for detecting MCI is around 90%. That’s a massive leap from the MMSE's sensitivity, which some studies have found to be as low as 18%.
Actionable Insight: This dramatic difference is the single most important factor when screening for early cognitive changes. A high false-negative rate, common with the MMSE in MCI cases, means missed opportunities for timely diagnosis, treatment planning, and support for patients and their families.
The clinical consequences are huge. If you use the MMSE on a patient with subtle memory complaints, you could end up sending them home with false reassurance. They might only return months or years later when their symptoms are more advanced and irreversible. In the same scenario, the MoCA would much more likely flag the issue, triggering the necessary follow-up.
How They Perform in Diverse Populations
The gap between the two tests gets even wider when you look at diverse populations, especially within the Canadian context. A person's cultural and educational background can have a big impact on their test performance, so a tool is only as good as its performance across different groups of people.
Research in Latin America and the Caribbean makes this crystal clear. One systematic review found that when screening Spanish-speaking populations for MCI, the MoCA had a sensitivity of about 90%, while the MMSE came in at a dismal 18%. This tells us the MoCA is far better at picking up early cognitive decline in these communities—a huge advantage given the rising rates of dementia.
These validation studies really highlight the MoCA's robust design. It's simply better suited for people with varied educational histories. It manages to maintain high sensitivity without a major drop in specificity, making it a more reliable and equitable screening tool. As we weigh these traditional screening methods, it’s also interesting to see how new technologies like AI for medical imaging and diagnostics are pushing the boundaries of what's possible, influencing sensitivity and specificity in profound new ways.
What This Means for Your Clinical Decisions
Let's walk through a practical example. Imagine a 65-year-old retired teacher from a rural community comes to your clinic worried about her memory. She has 12 years of formal education.
MMSE Scenario: You give her the MMSE, and she scores 27/30. This is considered "normal," so you might conclude her memory issues are just a part of normal aging.
MoCA Scenario: Instead, you administer the MoCA. She does well on orientation but has trouble with the clock drawing and the delayed recall of five words. Her final score is 23/30. After adding the one-point correction for her education level (≤12 years), her adjusted score is 24/30. This is below the typical cutoff of 26 and strongly suggests potential MCI.
This side-by-side comparison shows how the MoCA's superior sensitivity gives you a much clearer clinical picture, leading to a necessary referral for a full neuropsychological evaluation. That level of detail is vital for setting a baseline and tracking how things change over time. If you want to dive deeper into the importance of consistent measurement, our guide on test-retest reliability statistics is a great resource.
Ultimately, the MoCA’s psychometric strengths make it the clear winner for any clinician focused on catching cognitive impairment early.
Interpreting Scores and Applying Cut-Offs Accurately
Getting the raw score from a MoCA or MMSE is just the first step. The real clinical skill is knowing what that number means in the context of a whole person. While both tests are scored out of 30 points, those points tell different stories, especially when you factor in cut-off scores and demographic details.
The scoring itself is pretty direct. For the MMSE, a score of 24-30 is generally considered normal, 18-23 can suggest mild cognitive impairment, and a score below 18 points to something more significant. The MoCA, being a more sensitive tool, sets a higher bar: 26 or above is typically seen as normal. That higher threshold is a direct result of its power to pick up on more subtle cognitive issues.
But here’s the thing: just applying these standard cut-offs blindly can lead you down the wrong path. This is where the crucial work of score adjustment comes in, and it's something you can't afford to skip.
Adjusting for Education: A Critical Step
One of the biggest factors that can throw off a cognitive screener's results is a person’s level of formal education. Both the MoCA and MMSE can unintentionally penalize individuals with fewer years in school, which can easily lead to false positives.
To get around this, the MoCA has a simple adjustment built right in. The standard protocol is to add one point to the final score for anyone with 12 years or fewer of formal education. It's a small but powerful correction that helps level the playing field, making it more likely that a low score reflects a real cognitive change, not just an educational disadvantage.
Actionable Insight: A test score is not a diagnosis. It is a single piece of data that must be integrated with a patient's history, clinical presentation, and other relevant information. Over-reliance on a raw number, without considering factors like education or mood, can easily lead to misinterpretation.
This built-in adjustment is a huge differentiator between the two tests. It makes the MoCA a much more equitable and reliable tool across diverse populations. For a complete walkthrough of how to administer the test correctly, our guide provides detailed Montreal Cognitive Assessment instructions.
How Adjustments Impact Diagnostic Accuracy
Not adjusting for education isn't just a small oversight; it can have real clinical consequences. Practical Example: Imagine a 70-year-old patient with 10 years of schooling who scores a 25 on the MoCA. Without the adjustment, that score falls into the potential MCI range, which would understandably cause concern. But once you apply the one-point correction, their adjusted score becomes 26—placing them squarely in the normal range and changing the clinical picture completely.
Research right here in the CA region backs this up. Comparative studies have shown that education-adjusted scores dramatically improve the accuracy of both tools, but the MoCA still comes out on top. With proper adjustments, the MoCA achieved an accuracy of 87.8%, miles ahead of the MMSE's 71.1%.
The data also revealed the MoCA is more trustworthy for both confirming cognitive impairment (Positive Predictive Value of 84.5%) and, just as importantly, for ruling it out (Negative Predictive Value of 93.8%).
This evidence makes it clear: when interpreting scores, context is everything. The goal is to get a clean, accurate signal of someone's cognitive health, and applying the right adjustments is a non-negotiable step in getting there. By doing so, you can make more confident and precise decisions about who needs further evaluation.
When to Choose MoCA and When to Use MMSE
Translating test data into a confident clinical decision is what matters most when you're choosing between the MoCA and the MMSE. The right call isn't about which test is "better" in a vacuum; it’s about which one best fits the patient in front of you and the clinical question you need to answer. Real-world scenarios are the clearest way to see where each test truly shines.
Making the right choice at this early screening stage can significantly shape a patient's entire care journey. This simple decision tree shows how the MoCA's greater accuracy creates a more reliable clinical path compared to the MMSE.
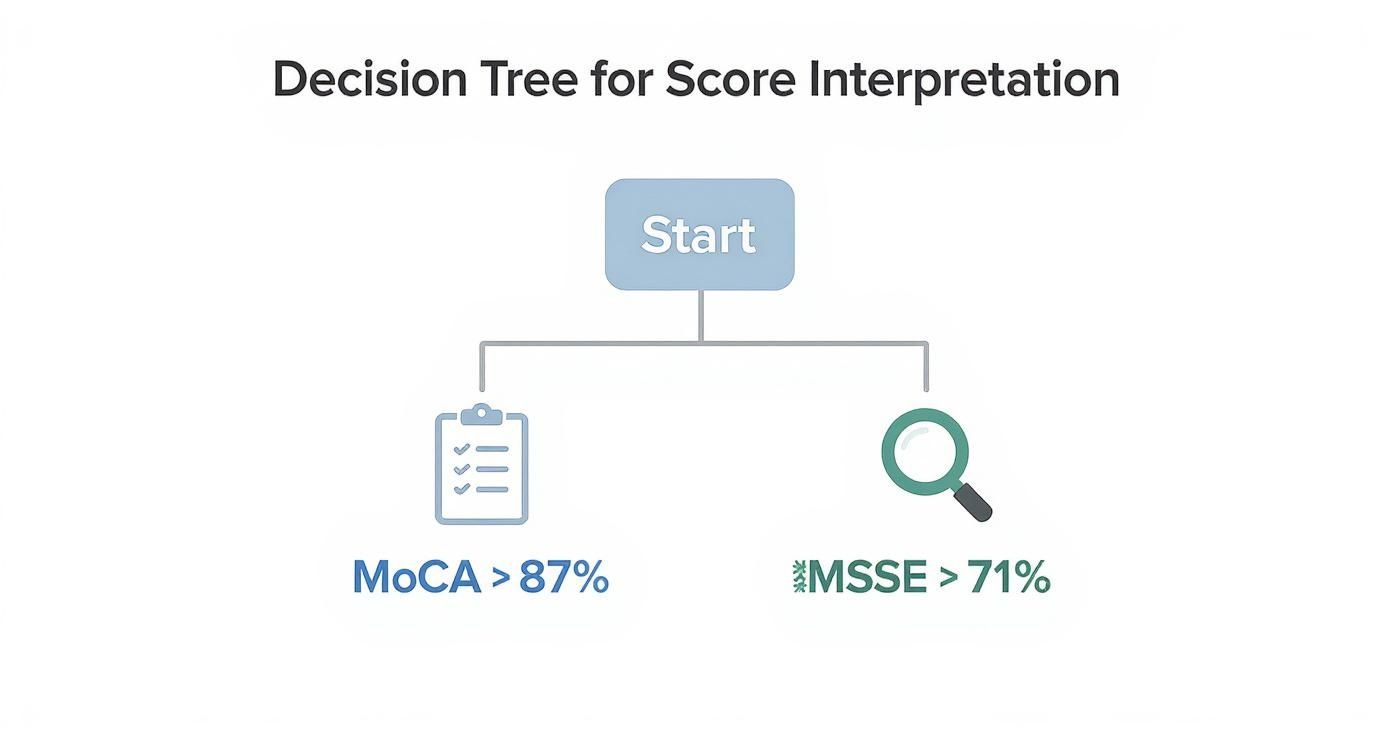
As you can see, the MoCA’s higher accuracy (>87%) makes it the clear starting point for uncovering subtle impairment. The MMSE, with its lower accuracy (>71%), is better suited for tracking more obvious, established cognitive decline.
When the MoCA is Essential
The Montreal Cognitive Assessment becomes your go-to screener when you suspect subtle deficits or have specific concerns about executive function. It’s built to succeed precisely where the MMSE is most likely to produce a false negative, giving you a false sense of security.
Think about these common clinical situations:
Highly Educated Professionals: Imagine a 60-year-old lawyer who reports some memory fuzziness but is otherwise high-functioning. Her years of education and cognitive reserve could easily allow her to max out the MMSE. The MoCA, with its tougher executive function and abstraction tasks, is far more likely to unmask the subtle deficits she's experiencing.
Suspected Early-Stage MCI: A family brings in their loved one, concerned about mild but persistent forgetfulness. In this scenario, the MoCA’s high sensitivity is critical for early detection, which opens the door for timely intervention. To better understand this crucial stage, you can read our guide on mild cognitive impairment vs dementia.
Post-Stroke or TBI Assessment: After a stroke or traumatic brain injury, assessing executive dysfunction isn't optional—it's essential. The MoCA’s Trail Making Test and verbal fluency tasks give you a direct window into these functions, which the MMSE completely misses.
Actionable Insight: If your clinical intuition points toward early or subtle cognitive change, the MoCA is almost always the right choice. It just gives you a much clearer, more nuanced picture of higher-order cognitive abilities.
When the MMSE May Suffice
Despite its well-known limitations, the Mini-Mental State Examination still has a role to play in certain contexts. Its speed and simplicity are its biggest assets, particularly when a deep dive isn't the immediate goal.
Here are a few scenarios where the MMSE remains a practical choice:
Tracking Moderate-to-Severe Dementia: For a patient with a confirmed diagnosis of Alzheimer’s disease, the MMSE can be a quick and easy tool to track the progression of their decline during routine follow-ups.
Initial Bedside Screening in Hospitals: In a busy acute care setting, time is everything. When the goal is a rapid screen for significant delirium or disorientation, the MMSE’s speed makes it a pragmatic option.
Populations with Very Low Education: For individuals with limited formal education or literacy, the MMSE’s simpler tasks may feel less intimidating. This can help establish an accessible baseline, though you'll still need to interpret the score with caution.
Research from our region backs up the MoCA's superior sensitivity. One study in Mexico found the MMSE identified only 26% of individuals with probable MCI. In contrast, the MoCA flagged 48.6% of them, powerfully demonstrating its strength in early detection. This is especially important in communities with diverse educational backgrounds, as test scores are so often influenced by years of schooling.
Moving Beyond Screening with Digital Cognitive Assessments
Deciding between the MoCA and the MMSE is a critical first step, but let's be honest, they are both just starting points. To truly integrate cognitive health into a modern clinical workflow, we have to look past these valuable but static paper-based tools. Clinicians are often up against time constraints, the hassle of manual scoring, and the sheer difficulty of tracking a patient's cognitive changes over time—all barriers that can blunt the impact of traditional screening.
This is where digital assessment platforms come in, offering a real solution to these everyday challenges. They make administration smoother, automate the scoring to cut down on human error, and—this is the big one—they make longitudinal tracking practically effortless. This changes the game, turning cognitive assessment from a single snapshot into a continuous, dynamic part of patient care.

Bridging the Gap From Screening to Ongoing Care
So, an initial MoCA or MMSE flags a potential concern. The immediate question every clinician asks is, "What now?" Digital platforms are the answer, creating a seamless bridge between that first screen and deeper, ongoing cognitive monitoring. Instead of a months-long wait for a full neuropsychological exam, you can start gathering more detailed data right away.
These tools provide objective, precise measurements across a much wider range of cognitive domains than any brief screener can. This richer dataset gives clinicians the confidence to make better-informed decisions, whether that means referring to a specialist or getting a care plan in motion.
The Power of Longitudinal Tracking
Perhaps the single greatest advantage of going digital is the ability to track cognitive function over time. A one-off test score is just a moment in time, but tracking performance over weeks, months, or years reveals the true trajectory of a patient's cognitive health.
Actionable Insight: Monitoring cognitive changes longitudinally is crucial for proactive care. It allows clinicians to detect subtle declines earlier, measure the effectiveness of interventions, and adjust treatment plans based on objective data rather than subjective reports alone.
Trying to manage this with paper tests is a logistical nightmare, riddled with practice effects and administrative headaches. Digital platforms, on the other hand, make it straightforward.
Objective Baselines: Establish a detailed cognitive baseline for every patient.
Regular Reassessment: Easily schedule automated follow-up assessments to watch for any changes.
Data-Driven Insights: See trends and patterns come to life through clear, intuitive reports.
Introducing a More Engaging Approach to Assessment
Let's face it: for many patients, traditional cognitive tests can be sterile and intimidating. Digital platforms like Orange Neurosciences completely change that experience. Our gamified, engaging activities feel less like a test and more like a set of brain-training exercises. This patient-friendly design helps lower testing anxiety and boost engagement, which ultimately leads to more reliable data.
Our platform is built to be the perfect next step after a MoCA or MMSE, providing the detailed follow-up needed for a complete clinical picture. In under 30 minutes, you get an objective profile covering key areas like attention, memory, and executive function.
This is how your practice moves beyond simple screening and into the world of proactive cognitive care management. By integrating our digital assessments, you can offer a more robust, data-driven strategy for patient monitoring, early detection, and personalized intervention.
Ready to see how a digital approach can elevate your clinical workflow? Explore how Orange Neurosciences provides the in-depth data you need to build on your initial MoCA or MMSE findings and deliver superior cognitive care.
Your Questions Answered: MoCA vs. MMSE
When deciding between the MoCA and the MMSE, clinicians often run into the same practical questions. Getting these sorted out is key to using these tools the right way in your practice.
Can You Just Swap the MoCA and MMSE?
Absolutely not. It's a common misconception, but they are built for different jobs. The MoCA is your go-to for sniffing out the subtle signs of mild cognitive impairment (MCI), while the MMSE is more of a yardstick for tracking decline in moderate to severe dementia.
Practical Example: a highly educated patient might breeze through the MMSE and score a 28/30, looking perfectly fine on paper. But the MoCA could reveal significant trouble with executive function, landing them a 24/30. If you'd used the MMSE, you would have missed a critical window for early intervention.
Actionable Insight: These tools serve completely different clinical purposes. The MoCA is for early detection of subtle problems. The MMSE is for monitoring more obvious cognitive loss. It’s the difference between using a magnifying glass and a wide-angle lens—you need the right tool for the view you're trying to get.
Does the MoCA Cost Anything or Require Certification?
Yes, there's a mandatory training and certification process to administer the MoCA, and it comes with a fee. This isn't just a hoop to jump through; it ensures that clinicians truly understand the test's specific scoring and administration rules, which is essential for getting trustworthy results.
While the test itself was free for clinical use in the past, policies can shift. Your best bet is to always check the official MoCA website for the latest on their licensing and fees.
How Often Should You Re-Screen a Patient?
There’s no one-size-fits-all answer here; it really depends on the person in front of you. For someone with a stable MCI diagnosis, checking in with the MoCA once a year might be enough to monitor for changes.
But for a patient recovering from a stroke, you’d want to assess more often—maybe at the three and six-month marks—to track their recovery or spot any new issues cropping up. The best approach is to get a solid baseline and then schedule follow-ups based on that individual’s condition and clinical journey.
What’s the Best Way to Document Results?
Good documentation is everything. Don't just jot down the final number. Always record the total score, plus any adjustments you made, like the one-point correction for education level.
Even more importantly, make notes on performance in specific areas. For instance, documenting that a patient scored 0/5 on delayed recall but did perfectly well on orientation gives you so much more to work with than a simple total score of 25/30. Those details are where the real clinical insights live.
Initial screening is just the first step. To get a richer, ongoing picture of your patient's cognitive health, see how the gamified digital assessments from Orange Neurosciences can fit into your workflow. Find out more at https://orangeneurosciences.ca.

Orange Neurosciences' Cognitive Skills Assessments (CSA) are intended as an aid for assessing the cognitive well-being of an individual. In a clinical setting, the CSA results (when interpreted by a qualified healthcare provider) may be used as an aid in determining whether further cognitive evaluation is needed. Orange Neurosciences' brain training programs are designed to promote and encourage overall cognitive health. Orange Neurosciences does not offer any medical diagnosis or treatment of any medical disease or condition. Orange Neurosciences products may also be used for research purposes for any range of cognition-related assessments. If used for research purposes, all use of the product must comply with the appropriate human subjects' procedures as they exist within the researcher's institution and will be the researcher's responsibility. All such human subject protections shall be under the provisions of all applicable sections of the Code of Federal Regulations.
© 2025 by Orange Neurosciences Corporation



