Essential guide to assessment for occupational therapy
Nov 6, 2025
Think of an assessment for occupational therapy as a personalized discovery process. It’s designed to get a clear picture of how someone's health or condition impacts their ability to do the things that matter most in their daily life. This is the crucial first step an occupational therapist (OT) takes to map out a client's strengths and challenges, setting the stage for a truly effective, client-centred plan.
The Foundation of Effective Occupational Therapy
You could say an OT is a bit like a detective for daily living. Their investigation always starts with a thorough assessment, which becomes the cornerstone for all successful therapy. This isn't just about running through a checklist or confirming a medical diagnosis; it's a deep dive into your unique world.
The main goal isn't just to see what you can't do. It’s to fully understand what you want and need to be able to do. That could be anything from cooking a meal and managing your finances to getting back to a hobby you love or feeling confident at work.
Building a Complete Picture
A comprehensive assessment for occupational therapy pieces together a holistic view of you as a whole person. It’s like building a detailed map that will guide the entire therapeutic journey. The process focuses on:
Identifying Strengths and Resources: Everyone has unique capabilities. The assessment shines a light on these existing skills, which can be leveraged during therapy. For instance, a client with memory issues might have fantastic organizational skills that can be used to build new routines.
Pinpointing Specific Challenges: This step clarifies exactly where and why difficulties are happening. Is it a physical limitation? A cognitive hurdle? An environmental barrier? Or maybe a mix of all three?
Understanding Your Environment: The assessment takes your physical and social surroundings into account. A home evaluation might show that simply rearranging furniture could prevent falls, or that a piece of assistive tech could make daily tasks manageable again.
This foundational step ensures the therapy is aimed squarely at what matters most.
An assessment is not about finding deficits; it's about discovering possibilities. It shifts the focus from a diagnosis to the individual's aspirations, creating a collaborative partnership between the therapist and the client from day one.
From Assessment to Actionable Goals
Once the OT has this complete picture, the next move is setting goals together. This isn't a one-sided decision. You and your therapist work as a team to establish clear, meaningful, and achievable objectives.
Here’s a practical example:
Imagine an older adult who is recovering from a fall and wants to keep living independently. The assessment might reveal they struggle with balance when reaching into high kitchen cabinets.
Instead of a vague goal like "improve balance," the collaborative goal becomes much more specific and functional: "Safely retrieve items from kitchen cabinets without losing balance or needing help."
This targeted approach, born directly from a detailed assessment, makes the therapy feel relevant and motivating. It connects every exercise and activity to a real-life outcome that directly improves quality of life. If you're curious about the wider scope of this profession, you can learn more about the practice of occupational therapy in Canada in our detailed guide.
Ultimately, this initial phase is what separates a generic plan from one that genuinely empowers you. By investing time in a thorough assessment, therapists ensure that the path forward is built on a solid foundation of understanding and shared purpose.
Standardized vs Non-Standardized Assessments
When an occupational therapist (OT) starts an assessment, they're not just picking a single tool; they're opening up a whole toolkit. Inside, you'll find instruments that fall into two main categories, and each one offers a unique and equally valuable window into your abilities and challenges. Understanding the difference between standardized and non-standardized assessments is the first step in seeing how OTs build a complete picture of your life.
Think of standardized assessments as using a ruler. They're tools designed to be given and scored the exact same way for everyone, every single time. This consistency delivers objective, data-driven measurements that can be compared against established norms—basically, the average results for a specific group, like people in your age range.
This structured approach takes the guesswork out of the equation. It provides a clear, quantitative baseline of a person's skills.
The Power of Objective Data
Standardized tools are absolutely vital for tracking progress. They also give OTs a common language—data—to communicate effectively with other healthcare professionals. They offer a reliable way to measure change over time and pinpoint specific areas where someone might be performing differently than their peers.
A great real-world example is the Bruininks-Oseretsky Test of Motor Proficiency (BOT-2). OTs often use this with children to get a precise read on their fine and gross motor skills. The child is asked to do a series of tasks, like balancing on one foot or tracing a line, and their performance is scored against a standardized set of criteria. The final score shows exactly where their motor skills stand compared to others their age.
For cognitive functions, tools like the Montreal Cognitive Assessment are go-to screeners for potential impairments. To see how these tools work in the real world, check out our guide on the Montreal Cognitive Assessment instructions.
The true power of standardized assessments is their ability to give an unbiased snapshot of function. They create a clear benchmark, which is essential for setting measurable goals and showing that therapy is actually working.
Capturing the Personal Story
While numbers and scores are important, they can't possibly tell the whole story. This is where non-standardized assessments shine. These tools are much more qualitative and flexible, built to capture the rich, personal context that a number on a test simply can't.
Think of these assessments as having a deep conversation or watching a home video. They can include methods like:
Skilled Observations: An OT might watch you do a simple daily task in your natural environment, like making a cup of tea in your own kitchen. This can reveal practical struggles and clever personal strategies that would never surface in a clinical setting.
In-depth Interviews: These are conversations that dive into your personal history, your values, and what you find meaningful. They help the therapist really get what your priorities are and what you hope to gain from therapy.
Checklists and Questionnaires: While some can be structured, they are often used to gather your subjective take on your experiences, preferences, and how you see your own abilities.
These methods add colour and depth to the black-and-white data from standardized tests, making sure the final therapy plan is truly built for you.
Here's a quick breakdown of how these two types of tools stack up:
Standardized vs. Non-Standardized Assessment Tools
Feature | Standardized Assessments | Non-Standardized Assessments |
|---|---|---|
Structure | Rigid, uniform administration and scoring. | Flexible and adaptable to the individual. |
Data Type | Quantitative (numbers, scores, percentiles). | Qualitative (observations, narratives, descriptions). |
Comparison | Compares an individual to a normative group. | Focuses on the individual's unique performance and context. |
Primary Use | Diagnosis, progress tracking, research, program eligibility. | Goal setting, understanding personal context, building rapport. |
Examples | BOT-2, Montreal Cognitive Assessment (MoCA), FIM. | Skilled observation, client interviews, checklists, COPM. |
Ultimately, the best approach uses both. By combining the objective data from standardized tools with the rich, personal insights from non-standardized ones, a therapist can create a truly holistic and effective plan.
Blending Both Worlds for a Complete View
The most effective OT assessments don't pit one type against the other; they skillfully blend them. One of the most powerful tools that does this beautifully is the Canadian Occupational Performance Measure (COPM).
Developed right here in Canada, the COPM is a unique semi-structured interview that puts you in the driver's seat, allowing you to identify and rate the importance of your own daily life challenges. It’s built on the idea that you are the expert on your life, and the tool respects that by letting you set the agenda. It perfectly blends the personal story of a non-standardized interview with a standardized scoring system that measures your own perception of your performance and satisfaction.
The use of evidence-based tools is widespread. In Canada, approximately 70% of OTs in acute care and 77% in inpatient rehabilitation use standardized assessments regularly. This just goes to show how essential these tools are for creating interventions that work. You can read more about the importance of OT competency in Canada to see how these practices are embedded in the profession.
By combining objective data with your personal story, therapists create a comprehensive and meaningful path forward. This balanced approach ensures that therapy focuses on what truly matters to you, all while being guided by solid evidence.
Taking a Look at the OT Assessment Process, Step by Step
The idea of an assessment for occupational therapy can sound a bit clinical and overwhelming, but it's really just a conversation that unfolds in stages. Think of it as a structured, yet deeply personal, journey designed to get from a place of uncertainty to a clear, practical plan. Let's walk through it together.
It all starts with a chat, not a test. Each step builds on the one before it, making sure the final roadmap is a true reflection of you—your needs, your goals, and your life.
Stage 1: The Referral and Getting the Lay of the Land
The first step is usually a referral, which might come from your doctor, another care provider, or even you. Once that’s in, the occupational therapist (OT) starts the important work of gathering your backstory. This isn’t just about filling out forms; it’s about getting to know your story before you even sit down together.
Your OT will look over your medical history, notes from other specialists, and the reason for the referral. This prep work means they walk into the first meeting with a solid foundation, making your time together more focused and productive right from the start.
Stage 2: The First Meeting and Making a Connection
That first face-to-face meeting is less about formal tests and more about building a connection. The real goal here is to establish trust and a sense of ease. Your therapist will create a comfortable space where you can open up about your experiences, your worries, and what you’re hoping to get out of therapy.
They'll put together an occupational profile, which is essentially a guided conversation about your daily life. They’ll ask about your routines, the different hats you wear (parent, employee, caregiver), your values, and your interests. This is your chance to paint a picture of what your world looks like and what activities truly matter to you.
This initial conversation is the heart of client-centred care. It ensures that the therapist sees you as a whole person, not just a diagnosis, and that your personal goals become the guiding star for the entire assessment process.
Stage 3: Picking the Right Tools for the Job
With a real understanding of who you are, the OT can now select the right assessment tools. As we’ve talked about, this is usually a mix of standardized and non-standardized methods to get a complete picture. The key is picking tools that directly connect to the goals and challenges you’ve already discussed.
Let's look at a practical example:
Say you’re a professional recovering from a concussion and find that managing your work emails has become overwhelming. Your OT might use a few different approaches:
Observation: The therapist might ask you to share your screen while you sort through a sample inbox. They'll watch how you organize messages, how long it takes to compose a reply, and if you seem fatigued by the screen.
Standardized Test: They could use a cognitive assessment online to get precise data on functions like attention and processing speed, which are critical for email management.
Interview: Afterwards, you’ll talk about it. They’ll want to know how you felt—were you frustrated, anxious, or did you get a headache?
This multi-pronged approach gives a rich, three-dimensional view of what’s really going on.
Stage 4: Making Sense of It All
Once all the information is gathered, the therapist’s job is to put the puzzle pieces together. They blend the hard data from tests with the real-life insights from observations and conversations. They’re looking for patterns, connecting the dots, and forming a professional view of your strengths and the specific barriers holding you back.
This analysis is what turns raw information into a meaningful clinical picture. It helps answer the big question: "Why is this specific activity so hard, and what can we do about it?"
Stage 5: Teaming Up on Goals and a Plan
This is the most important part. You and your therapist sit down together to review everything. They’ll explain what they found in clear, simple language, and together, you'll set meaningful, achievable goals.
This isn't a one-way street where the therapist hands you a plan. It's a partnership. Your priorities drive the whole process. Going back to our email management example, a collaborative, actionable goal might sound like this: "To be able to process 20 work emails in 30 minutes using a new organizational strategy without getting a headache."
From that specific goal, you'll build an intervention plan together, outlining the exact strategies, exercises, and supports that will help you get there. You’ll leave the assessment feeling like you have not just answers, but a clear, hopeful, and actionable path forward. To discover more about the digital tools transforming these assessments, please explore our comprehensive guide on the future of cognitive assessment online.
How OT Assessments Change Lives in the Real World
The true value of a detailed assessment for occupational therapy isn't found in scores or reports. It's in the real-world changes it sparks. This is where theory gets put into practice, and a therapist's careful analysis helps someone reclaim their independence, confidence, and joy. These stories show how the right assessment tools build a bridge to practical, life-altering solutions.
This visual captures the simple yet powerful flow from the initial referral and deep-dive assessment to the creation of a truly personalized intervention plan.
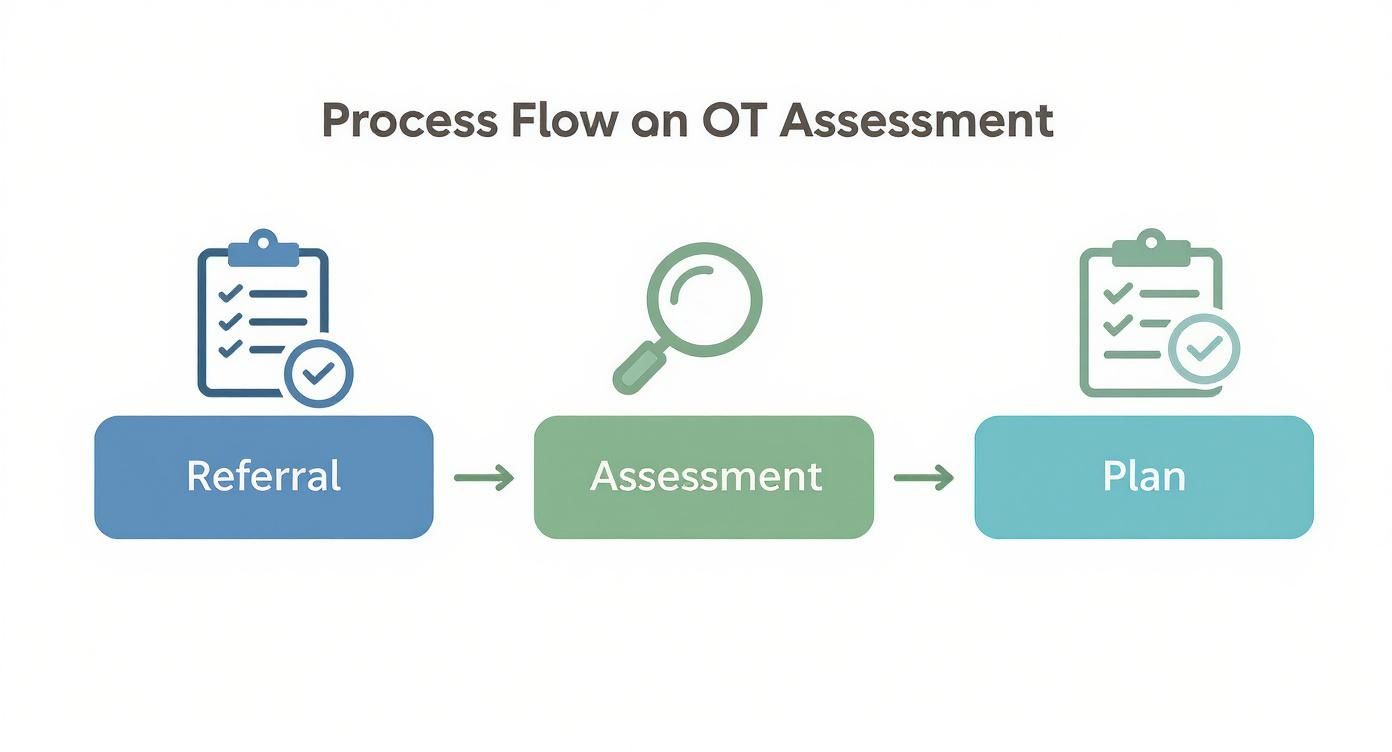
As the infographic shows, each step logically builds on the last. This ensures the final plan is directly shaped by the thorough discovery process of the assessment phase.
Enabling Independence After a Stroke
Let's start with Robert, a 78-year-old who just came home after a stroke. Medically, he was stable, but his confidence was completely shattered. He lived in fear of falling and worried he'd become a burden, making simple tasks like getting out of a chair feel like climbing a mountain.
His occupational therapist began with two key assessments:
The Berg Balance Scale: This standardized test gave them hard data on Robert's balance during a series of specific movements, confirming a high risk of falling.
A Home Safety Evaluation: This was a non-standardized assessment. The therapist simply watched Robert move through his own home, spotting real-world hazards like loose rugs and poor lighting in the hallway.
The findings from this blended approach led directly to a practical, actionable plan. The therapist recommended simple but powerful home modifications, like installing grab bars in the bathroom and adding non-slip mats to the shower. They also designed a targeted exercise program based on his Berg Balance score to steadily rebuild his strength and stability.
The Actionable Insight: The assessment revealed that Robert's fear was as significant a barrier as his physical imbalance. The plan addressed both, giving him tangible safety tools (grab bars) to build psychological confidence while he worked on his physical strength.
Improving Focus in the Classroom
Now, think about Maya, a bright seven-year-old who couldn't seem to stay focused in her busy classroom. She was constantly out of her seat, easily distracted by noise, and struggled to finish her work. It was causing her to fall behind, and both she and her teacher were feeling the frustration.
An occupational therapist came in to conduct an assessment focused on sensory processing. The therapist used a combination of tools to get to the root of Maya's unique sensory needs:
The Sensory Profile: This standardized questionnaire, filled out by Maya's parents and teacher, painted a clear picture: she was highly sensitive to both sounds and sights.
Direct Classroom Observation: The therapist spent time watching Maya in her learning environment, noticing how she’d flinch at loud announcements over the intercom or squint under the harsh fluorescent lights.
This narrative shows that an assessment for occupational therapy is fundamentally about understanding a person's experience of the world. By seeing the classroom through Maya's eyes, the therapist could pinpoint the exact environmental triggers causing her distress.
The insights from the assessment led to targeted strategies that made an immediate difference. The therapist worked with the teacher to create a "quiet corner" in the classroom where Maya could go when she felt overwhelmed. She was also given a weighted lap pad for calming pressure and noise-cancelling headphones to use during independent work.
The Actionable Insight: The assessment identified that Maya's behavior wasn't a choice, but a reaction to sensory overload. The solution wasn't to change Maya, but to adapt her environment. These simple tools empowered her to self-regulate, giving her control over her learning experience. You can learn more about how Orange Neurosciences supports neurodiverse learners on our blog.
The Future of OT Assessments Technology and AI

The world of occupational therapy is changing fast, and technology is at the helm. It’s pushing the assessment for occupational therapy to be more precise, engaging, and frankly, more accessible than it’s ever been. We’re finally moving beyond just paper-based tests and into a world of dynamic digital platforms that measure cognitive and motor skills in truly interactive ways.
This opens up a whole new world for therapists and clients. Think about it: instead of static questionnaires, we now have assessments that feel more like intuitive games. They can capture thousands of data points on functions like attention, memory, and processing speed—often without the client even feeling like they're being tested.
The Rise of AI-Powered Gamified Tools
One of the most exciting shifts is how artificial intelligence (AI) and gamification are being woven into the assessment process. These aren’t just video games; they are incredibly sophisticated clinical tools built to capture the kind of precise data that older methods could easily miss.
Pioneers like Orange Neurosciences are leading this charge. They use game-like activities to measure complex cognitive functions in a way that feels natural. For example, a task might look like a simple matching game on the surface, but behind the scenes, it's tracking reaction time, decision-making speed, and visual-motor coordination with millisecond accuracy.
This approach brings two huge wins to the table:
Deeper Insights: AI algorithms can dig into performance patterns, giving therapists a much richer picture of a client's cognitive profile. This helps pinpoint specific areas that need targeted intervention.
Improved Client Engagement: Whether for a child or an adult, a gamified assessment is far less intimidating and often more fun than a standard test. This leads to more authentic, reliable performance data.
By transforming the assessment experience, these tools not only deliver better data but also foster a more positive and motivating therapeutic environment from the very first interaction.
Breaking Down Barriers with Telehealth
Technology is also making OT assessments reachable for more people. Telehealth has become an essential part of modern healthcare, knocking down geographical barriers and bringing expert care to remote and underserved communities across Canada.
A therapist in Toronto can now run a detailed cognitive or functional assessment with a client living hundreds of kilometres away. This is a game-changer for making sure everyone gets timely, effective care, no matter where they live. And the workforce is growing to meet this need. In 2023, Canada had over 20,000 registered occupational therapists, a jump that reflects how vital OTs are becoming in all kinds of settings, including telehealth. You can see the full breakdown in the Canadian Institute for Health Information report.
What This Means for You
All these advancements are making the assessment for occupational therapy a more collaborative, data-driven, and personalized experience. Whether it's AI helping us understand the brain or telehealth connecting a therapist to a client, technology is empowering everyone involved. You can explore how Orange Neurosciences' solutions are integrating these technologies to shape what's next in cognitive care.
And we're just scratching the surface. Immersive technologies like virtual reality are on the horizon, promising even more realistic assessment scenarios. To get a sense of how these tools are already changing healthcare education and setting the stage for OT, check out this guide on virtual reality for medical training. These tools aren't just improving assessments—they're building a more hopeful and effective path toward recovery and well-being.
How to Find the Right Occupational Therapist for You
Deciding to start your therapy journey is a big step, and finding the right professional to guide you is just as important. When you know where to look, locating a qualified occupational therapist in Canada is actually pretty straightforward. It's all about connecting with a provider who can become a true partner in your care.
So, where do you start? Your first stop should be your province's regulatory body. These organizations keep official registers of all licensed OTs, which guarantees that anyone you find is fully qualified and held to high professional standards. Another fantastic resource is the Canadian Association of Occupational Therapists (CAOT), which has a helpful "Find an OT" tool on its website. This can help you narrow down therapists in your area who specialize in what you need.
Questions to Ask a Potential Therapist
Once you have a shortlist, it's time to see who feels like the best fit. A quick phone call can reveal a lot about a therapist's personality and approach. You're looking for someone who is collaborative and puts you at the centre of the process.
To get a good sense of their style, try asking a few key questions:
What does your typical assessment for occupational therapy involve?
How do you make sure clients are actively involved in setting their own goals?
What's your experience with [mention your specific condition or challenge]?
This isn't an interrogation; it's a conversation. It's your chance to see if their assessment style feels right for you. A great therapist will make you feel heard and respected from the very first chat. Their answers should give you the confidence that they're focused on understanding your unique story and priorities.
Finding the right OT goes way beyond credentials—it's about finding a collaborative partner. The best therapeutic relationships are built on a foundation of trust, open communication, and a shared commitment to your goals.
To keep up with the growing demand for OTs, Canada also welcomes skilled professionals from all over the world. A program called the Substantial Equivalency Assessment System (SEAS) helps internationally educated occupational therapists get licensed to practice here. In recent years, British Columbia and Ontario have seen the biggest influx of these talented practitioners. You can read more about how these professionals are strengthening the OT workforce in Canada/4920535/839226/article.html).
By using these resources and asking the right questions, you can find a provider who will support you every step of the way. To see how our client-centred, AI-powered assessments can support your journey, visit our website or contact our team to learn more.
Frequently Asked Questions
It’s completely normal to have questions when you’re exploring the world of occupational therapy. To help you feel more prepared, we’ve put together clear, straightforward answers to a few of the most common ones we hear.
Think of this as a quick guide to help you feel more confident as you get started.
How Long Does an OT Assessment Usually Take?
There really is no one-size-fits-all answer here, because every assessment for occupational therapy is shaped around the individual. For a more straightforward situation, a single session of about 60 to 90 minutes might be all that's needed to get a clear picture.
But for more complex cases, say, where we need to see how things are going at both home and school, the assessment might be spread over a few sessions. This approach gives the therapist a complete understanding without overwhelming anyone.
Are OT Assessments Covered by Provincial Health Insurance in Canada?
This is a big question, and the answer can vary quite a bit across Canada. It all depends on your province and your specific situation.
Often, if you receive OT services inside a hospital or a public rehabilitation centre, your provincial health plan will cover it. For private clinics, however, payment is usually out-of-pocket or covered by a private health insurance plan. The best first step is always to check directly with your provincial health authority and your insurance provider to see exactly what your coverage looks like.
What Should I Expect After the Assessment Is Finished?
The end of the assessment is really the beginning of a partnership. You won't just be handed a stack of papers. Your therapist will sit down with you and walk through all the findings in plain, easy-to-understand language.
The post-assessment meeting is a partnership. It's where clinical findings are translated into a shared vision for the future, ensuring your personal goals are the driving force behind the intervention plan.
Together, you'll work through a few key steps:
Review a Summary Report: This document breaks down your strengths, the challenges you're facing, and the therapist’s clinical thoughts.
Set Meaningful Goals: This is a team effort. You’ll decide on clear, achievable goals based on what’s most important to you and your family.
Develop an Intervention Plan: You'll map out the specific therapies, strategies, and supports that will help you reach those goals.
This way, you’re an active, informed participant in your own care right from the start. As a side note for practitioners and patients looking for instant information, it can be useful to enhance user support with a chatbot for FAQs to provide immediate answers.
Ready to take the next step toward a clearer cognitive picture? At Orange Neurosciences, we use advanced, AI-powered tools to make the assessment process more precise and engaging. Discover how our evidence-based platform can support your journey by visiting us at https://orangeneurosciences.ca.

Orange Neurosciences' Cognitive Skills Assessments (CSA) are intended as an aid for assessing the cognitive well-being of an individual. In a clinical setting, the CSA results (when interpreted by a qualified healthcare provider) may be used as an aid in determining whether further cognitive evaluation is needed. Orange Neurosciences' brain training programs are designed to promote and encourage overall cognitive health. Orange Neurosciences does not offer any medical diagnosis or treatment of any medical disease or condition. Orange Neurosciences products may also be used for research purposes for any range of cognition-related assessments. If used for research purposes, all use of the product must comply with the appropriate human subjects' procedures as they exist within the researcher's institution and will be the researcher's responsibility. All such human subject protections shall be under the provisions of all applicable sections of the Code of Federal Regulations.
© 2025 by Orange Neurosciences Corporation



